Virus-inhibitory activity of the antigen complex of opportunistic pathogenic bacteria against SARS-CoV-2
- Authors: Svitich O.A.1, Nagieva F.G.1, Kurbatova E.A.1, Barkova E.P.1, Kharchenko O.S.1, Stroeva A.D.1, Pashkov E.A.1, Lisakov A.N.1, Gracheva A.V.1, Potapova M.B.2, Faizuloev E.B.1, Zverev V.V.1
-
Affiliations:
- I. Mechnikov Research Institute of Vaccines and Sera
- I.M. Sechenov First Moscow State Medical University (Sechenov University)
- Issue: Vol 100, No 2 (2023)
- Pages: 143-152
- Section: ORIGINAL RESEARCHES
- URL: https://microbiol.crie.ru/jour/article/view/1251
- DOI: https://doi.org/10.36233/0372-9311-309
- EDN: https://elibrary.ru/swcktv
- ID: 1251
Cite item
Abstract
Introduction. The antigen complex of opportunistic pathogenic bacteria (ACOPB) has a protective effect against avian influenza viruses, herpes virus type 2, and other viruses that cause acute respiratory viral infections. In the context of the COVID-19 pandemic, an important task is to find out whether ACOPB has a protective effect against SARS-CoV-2.
The purpose of the study was to evaluate in vitro the ACOPB virus-inhibitory activity against the Dubrovka laboratory strain of SARS-CoV-2.
Materials and methods. The study was performed using Vero cell line CCL-81, human peripheral blood mononuclear cells (PBMCs), mouse monoclonal anti-idiotypic antibodies structurally mimicking biological effects of human interferons (IFNs), the Dubrovka laboratory strain of SARS-CoV-2. The infectivity of the virus was assessed by two methods: by virus titration using cell cultures and the limiting dilution method when the results are assessed by a cytopathic effect; the second method was a plaque assay. The in vitro virus inhibition test was performed using the cell culture susceptible to SARS-CoV-2; the mixture containing a specific dose of the virus and a two-fold dilution of ACOPB was transferred to the cell culture after the ACOPB medication had interacted with the virus at 4ºC for 2 hours. The ACOPB virus-inhibitory activity against SARS-CoV-2 was assessed by the functional activity of α/β and γ IFN receptors (RIFN) in human PBMCs induced in vitro by ACOPB and the ACOPB mixture with the specific dose of SARS-CoV-2. The RIFN expression level was measured by the indirect membrane immunofluorescence test.
Results. Hemagglutination assay using chicken, mouse, guinea pig, and human red blood cells was performed for detection of the SARS-CoV-2 inhibitory protein. The lysate of Vero CCL-81 cells infected with SARS-CoV-2 Dubrovka demonstrated the highest hemagglutination activity with guinea pig red blood cells and low titers of hemagglutination in the virus-containing fluid. The virus inhibition test in the Vero CCL-81 cell culture demonstrated that ACOPB inhibited 10 doses of SARS-CoV-2 Dubrovka with the titer 1 : 32, providing 100% protection of the cell culture for 8 days (the monitoring period). ACOPB induced α/β and γ RIFN expression on membranes of human PBMCs in in vitro cultures and decreased RIFN α/β and γ expression after its interaction with SARS-CoV-2 Dubrovka.
Conclusion. The experimental studies including the virus inhibition test in the cell culture susceptible to SARS-CoV-2 Dubrovka and the indirect membrane immunofluorescence assay using monoclonal anti-idiotypic antibodies mimicking IFN-like properties demonstrated that ACOPB had both an immunomodulatory and a virus-inhibitory effect.
Full Text
Introduction
In the past few decades, a significant breakthrough has been made in the studies of cellular and molecular mechanisms of immunity. The previously established views of the role played by innate immunity in resistance to a wide range of pathogens and in activation of the adaptive immunity have been revised. It has been found that some bacterial antigens (lipopolysaccharides, peptidoglycans, protein antigens on the cell wall, etc.) are involved in controlling the innate immunity system [1, 2].
Activation of TLR-mediated mechanisms of innate immunity through ligands of Toll-like receptors triggers protection against different pathogens. The antigen complex of opportunistic pathogenic bacteria (ACOPB) is used for activation of innate immunity and protection against viral infections. Previous studies assessed the ACOPB protective effect against avian influenza virus serotype H5N2 and herpes virus type 2 [3–5]. ACOPB is used for prevention and treatment of acute respiratory infections, chronic inflammatory diseases of upper and lower respiratory tract, bronchial asthma, atopic dermatitis, pollinosis, latex allergy, etc. Clinical trials showed that immunotherapy including ACOPB, together with the background therapy, resulted in improvement of the phagocytic activity of peripheral blood mononuclear cells (PBMCs), and increased the synthesis of interferons (IFN)-α and -γ, etc. [6–9].
SARS-CoV-2 is responsible for the coronavirus infection that caused the pandemic in 2019. Severe disease and fatal outcomes resulting from this infection are associated with damage to the lungs, cardiovascular system, kidneys, and central nervous system. Significant efforts are being made to create antiviral therapeutic and preventive medications [10–12].
The purpose of the study was to evaluate in vitro the ACOPB virus-inhibitory effect against SARS-CoV-2 Dubrovka.
Materials and methods
The study was performed using strains from the collection of the common use center of the Mechnikov Research Institute of Vaccines and Sera, with funding from the Ministry of Science and Higher Education of the Russian Federation (Agreement No. 075-15-2021-676 of 28/7/2021).
ACOPB is a next-generation medication representing a complex of antigens activating expression of receptors in cells of the innate immunity system (Toll-like receptors 1/2, 4, 5, 2/6, 9), thus providing its effectiveness against a wide range of pathogens and allergy. The medication was created using antigenic components extracted from Staphylococcus aureus, Klebsiella pheumoniae, Proteus vulgaris, Escherichia coli.
Cell cultures
The study was performed using the continuous green monkey kidney-derived Vero CCL-81 cell line from the American Type Culture Collection. Cells were grown in the DMEM/F12 basal medium (PanEco) supplemented with 5% fetal bovine serum (FBS; HyClone) and 40 µg/ml of gentamicin.
PBMCs were collected from O-positive donors. The study was performed with voluntary informed consent of the participants.
Monoclonal anti-idiotypic antibodies to IFN-α and -γ receptors (RIFN) were obtained by injecting mouse lymphatic hybridomas producing antibodies with an internal image of human IFN-α/β and -γ to syngeneic BALB/c mice, which was followed by collection and purification of ascitic fluid containing the above antibodies [14, 15].
SARS-CoV-2 coronavirus
The SARS-CoV-2 Dubrovka virus was obtained by isolating the virus in the Vero cell culture from the clinical specimen. For this purpose, we used an oropharyngeal swab collected from a 61-year-old female patient, in which the real-time RT-PCR detected a high level of SARS-CoV-2 RNA (8.82 lg TCD50/ml). Later, the patient developed clinical symptoms of COVID-19: cough, shortness of breath, fever, loss of taste and smell. The thoracic CT showed typical lung tissue consolidation with the total affected area from both sides reaching 50%, and the patient was diagnosed with COVID-19, virus identified (U07.1, ICD-10); community-acquired bilateral polysegmental viral pneumonia. The test was performed with the patient’s voluntary informed consent.
The Vero cell culture was infected with clinical material and incubated in the CO2 incubator for 5 days until reaching the cytopathic effect (CPE) manifested by cell rounding; then, the next passaging was performed. To identify the virus, the material obtained at different passaging levels was tested for the presence of SARS-CoV-2 RNA using the real-time reverse transcription polymerase chain reaction and primers for the N gene. At the 2nd, 7th, 14th, and 21st passages, high levels of SARS-CoV-2 RNA (9.0, 9.7, 9.2, and 9.9 lg RNA copies/mL, respectively) were detected in the culture liquid. The isolate was assigned to species SARS-CoV-2 (clade GH) by sequencing the S gene (GenBank accession number MW514307) [13].
The virus infectivity was measured by two methods: the limiting dilution in cell cultures grown in 48-well plates (Thermo Scientific/Nunc) based on CPE and the plaque assay (PFU50) [18] in our modification. Both methods used for measuring the infectivity of viruses causing CPE in the cell culture, which is manifested by cell rounding, should be confirmed by another method of virus infectivity assessment to differentiate CPE from apoptosis.
Tenfold dilutions of the virus-containing fluid (VCF) were prepared starting from dilution 10–1 to 10–8 using the DMEM basal medium with 2% FBS. The growth medium was removed from 48-well plates with the Vero CCL-81 cell monolayer; the cell monolayer was washed one time with Hanks’ solution. Then, 0.2 ml of each VCF dilution was dispensed into 6 wells of the plate; 0.2 ml of basal medium was dispensed into the control wells. The interaction between VCF and the cells continued in an incubator for 1 hour at 36.5ºC and 5% CO2. After the interaction was over, 0.8 or 0.9 ml of basal medium (the serum-free DMEM medium) was added to each well, including wells with control cells.
The titration results were assessed on the 4th–5th day from the infection of the cell culture. The virus titer was expressed as the highest virus dilution causing CPE in 50% of infected cell cultures in the absence of cell destruction in the uninfected cell cultures.
Prior to the plaque assay, the Vero CCL-81 cell culture was grown in the growth medium in 12-well plates. 24–48 hours after a confluent cell monolayer had been formed, the medium was removed; the cell monolayer was washed with Hanks’ solution. 0.1 ml or 0.2 ml of tenfold VCF dilutions were dispensed into 3 wells, into the central area. One well was left uninfected for cell culture control. The contact between the virus and the cells continued in an incubator for 1.5 hours at 36.5ºC and 5% CO2. The remaining liquid was removed from all the wells, including the control well, and 2 ml of agar overlay consisting of 0.5% Noble agar and DMEM medium with 4% FBS was added to each of them. After the agar overlay had solidified at room temperature, the plates were incubated in the incubator at 36.5ºC and 5% CO2. On the 5th day, 1 ml of 10% trichloroacetic acid solution or 3% paraformaldehyde solution was dispensed onto the agar overlay and the plates were incubated in the incubator for 1 hour. After the cells had been fixed, the agar overlay was removed by shaking; the cell monolayer was washed with water; the tray was dried, and 1 ml of 0.1% gentian violet solution was dispensed into wells and remained there for 2–3 min. Then, the tray was washed with running water and dried. The number of plaques was counted for each well. The average number of plaques from 3 wells for each virus dilution was calculated. The virus titer was expressed as logarithms PFU50/0.1 ml, using the formula:
X = A × B/0.2,
where X is a titer in PFU per 1 ml; A is the average number of plaques; B is the virus dilution; 0.2 — the amount of inoculum (ml) dispensed into one well.
Hemagglutination assay
Hemagglutination is defined as the ability of some viruses to agglutinate red blood cells in certain mammalian and avian species. Viruses exhibit their hemagglutination properties selectively toward red blood cells of certain animal species. Some viruses can affect a wide range of animal species, while other viruses can affect only a limited range of species. There is a relationship between infectivity and hemagglutination properties of the virus. The source of the virus is important for the results of the hemagglutination assay (HA). The hemagglutination properties of the virus are not displayed in any virus-containing material. For example, using HA, the influenza virus can be detected in nasopharyngeal washes from a sick person (occasionally), in embryonic tissue cultures, and in suspensions of infected mouse lungs [16].
HA was used for detection of the presence or absence of viral hemagglutinin in cells infected with SARS-CoV-2 and in VCF. For this purpose, we used for types of red blood cells: chicken, mouse, guinea pig, and human. The test involved agglutination of red blood cells by the viral hemagglutination antigen. HA was performed in round-bottom 96-well plates (SPL Life Sciences, Ltd.) and included twofold dilution of antigens in 100 µl of saline solution and adding of the equal amount of 0.25% red cell suspension to each dilution. The specimens remained exposed to red blood cells at 4ºC for 1.0–1.5 hours until red blood cells settled down in the control wells; then, the HA results were assessed. The hemagglutination titer of the virus was expressed as the highest dilution of the antigen, at which agglutination was observed.
Virus replication inhibition test
Many species of microorganisms produce biological compounds that can affect viruses. For example, spore-forming bacteria Bacillus pumilus, when grown in the optimum NEW medium, produce biologically active compounds characterized by antiviral activity against enteroviruses (poliovirus type 1, Coxsackie B virus (1–6), ECHO-3, and ECHO-6 [17].
The test procedure was selected for ACOPB to assess its extracellular virucidal action in vitro toward SARS-CoV-2. Prior to that, it was found that ACOPB did not demonstrate any virucidal action in vitro toward 100 doses (2.5 lg PFU50/0.2 ml SARS-CoV-2 with a virus titer of 4.55 lg PFU50/0.2 ml).
The virus replication inhibition (VRI) test was performed using two 24-well plates with the Vero CCL-81 cell monolayer. One plate was used for the VRI test; the other plate was used for SARS-CoV-2 titration. The serum-free DMEM medium was used for twofold dilutions of ACOPB (dilutions from 1 : 2 to 1 : 32). SARS-CoV-2 was added to each dilution in the amount equal to 10 doses (3.5 lg TCD50/0.2 ml or 3.55 lg PFU50/0.2 ml at the virus titer of 4.5 lg TCD50/0.2 ml and 4.55 PFU50/0.2 ml). ACOPB interacted with the virus at 4ºC for 2 hours, including regular shaking of ingredients. After the interaction was over, each dilution of the medication and virus mixture in the amount of 0.2 ml was dispensed into a 24-well plate, which was washed one time with Hanks’ solution. Each dilution of the mixture was transferred into 4 wells of the plate, while 2 wells were designated for cell control and the other 2 wells — for control of 10 doses of the virus. The virus interacted with the cells in the incubator at 5% CO2 for 1.5 hours; then, DMEM basal medium in the amount of 0.8 ml was added to all the wells in 24-well plates and the culturing continued. After the lytic cell destruction in the control well with 10 doses of the virus was detected (usually on the 2nd–3rd day after the infection), the results of the VRI test were assessed. The VRI test titer was expressed as the highest dilution of the medication, at which we observed 100% protection of cells against SARS-CoV-2.
Indirect membrane immunofluorescence assay
PBMCs were isolated from heparinized venous (20 U/ml) human blood using the Ficoll density gradient centrifugation (1.077 g/cm3) (PanEco) for 25 minutes at 1500 rpm. A cell fraction was selected and washed three times with pre-cooled phosphate-buffered saline; the remaining cells were resuspended in the DMEM/F12 medium with 2% FBS so that there were not less than 1 mln lymphocytes in each well. The suspension of lymphocytes in the amount of 1 ml was transferred into wells of 12-well plates.
Two hours before isolation of lymphocytes from venous blood, the equal amount of 10 doses of SARS-CoV-2 was added to 0.2 ml of twofold dilutions of ACOPB and left for interaction at 4ºC, with regular shaking of the mixture.
Three dilutions (1 : 10, 1 : 20, and 1 : 40) of ACOPB in the amount of 0.1 ml and the ACOPB and SARS-CoV-2 mixture in the amount of 0.1 ml were dispensed into wells of 12-well plates with lymphocytes. Then, samples of lymphocytes were collected from the wells at different time intervals, starting from 1 hour, in the amount of 5 µl (3 samples per each time interval) and applied uniformly to chamber slides; the cell samples were left to dry out at room temperature overnight. Then, the samples were fixed with double-filtered 3% paraformaldehyde supplemented with 0.2% bovine serum albumin for 1 hour at room temperature. Then, they were washed two times with phosphate-buffered saline and were blocked in 10% normal goat serum for 1 hour. Mouse monoclonal anti-idiotypic antibodies for IFN-α/β and -γ were applied to each chamber with samples in the amount of 20 µl and incubated in the humidified chamber for 1 hour at 36.5ºC in the thermostat. After the interaction with antibodies, double washing and drying, the working solution of anti-mouse FITC conjugate (BioRad) was applied to the samples. Then, they were incubated in the humidified chamber for 1 hour. Prior to its application, the FITC conjugate was diluted in 0.1% saponin solution with Hanks’ solution and 0.01 M HEPES-buffered saline. After the interaction between the samples and the conjugate was over, the slides were washed twice with Hanks’ solution and dried.
The expression level of RIFN-α/β and -γ in PBMCs was measured using the Optica fluorescent microscope (Italy) with 100X oil immersion objective and 10X eyepiece by the percentage of luminescent lymphocytes per 200 analyzed cells (repeated for each time interval).
VCF was treated according to E. Norrby [19]. Tween 80 diluted 1:10 was added to 100 ml of VCF in the amount of 2 ml. The mixture was shaken on ice for 5–10 minutes. Ether was added to the mixture in the amount equal to 1/2 of the volume of the mixture. The mixture was shaken for 15–20 minutes and then centrifuged for 20 minutes at 3000 rpm. After the centrifugation, the mixture separated into layers; the cloudy film at the top was carefully pierced with a pipette, trying not to stir it up, and the lower layer was aspirated. The solution was placed in a flask with a cotton-gauze plug to allow ether to evaporate and remained there for 24 hours at room temperature. Then, the hemagglutination titer of the antigen was measured; the solution was dispensed into vials (1.0 ml) and dried. The dried antigen can be stored in a refrigerator for several years without loss of activity. The culture liquid containing uninfected cells and prepared using the same technique was used as a control medium.
Statistical analysis of the data
The statistical significance of the obtained data was assessed using the Mann-Whitney U-test. The difference was considered significant at p ≤ 0.05. The reliability was measured using the GraphPad Prism 4 software (Graph Red).
Safety requirements
All works involving SARS-CoV-2 were performed in compliance with the safety requirements applicable to handling hazard group 3 pathogens. All the employees working with the virus were briefed on safety precautions and have valid certificates for qualification in Bacteriology, Virology, Biological Safety, which were issued by the Russian Research Anti-Plague Institute “Microbe” of Rospotrebnadzor.
Results
During the 1st stage of the study, we conducted tests checking for the presence or absence of hemagglutination properties of SARS-CoV-2 Dubrovka. HA was used to study hemagglutination properties of the virus toward chicken, mouse, guinea pig, and human red blood cells using the suspension of Vero CCL-81 cells infected with SARS-CoV-2 Dubrovka and VCF from the infected cells.
The results presented in Table 1 clearly demonstrate the hemagglutination properties of SARS-CoV-2 Dubrovka in the infected cells and low titers in VCF, which can be explained by a low content of hemagglutinin or by non-specific masking of the phenomenon. The highest hemagglutination activity is manifested in the lysate of infected cells with guinea pig red blood cells.
Table 1. Hemagglutinating activity of SARS-CoV-2 Dubrovka
Studied specimens | Virus titer in HA with 0.25% suspension of red blood cells | |||
chicken | mouse | guinea pig | human | |
Lysate of infected Vero CCL-81 cells | 1 : 64 | 1 : 16 | ˃ 1 : 256 | 1 : 32 |
VCF from Vero CCL-81 cells | 1 : 16 | 1 : 2 | 1 : 2 | 1 : 2 |
Uninfected Vero CCL-81 cells | 0 | 0 | 0 | 0 |
Red blood cell control | 0 | 0 | 0 | 0 |
The HA results show that Vero CCL-81 cell lines infected with SARS-CoV-2 Dubrovka contain viral hemagglutinin — one of the major viral proteins that are targets for antiviral agents.
For the VRI test, it is important to determine the dose of SARS-CoV-2 Dubrovka, which should be used with the ACOPB antiviral medication for VRI. The infectious dose of the virus was identified using the limiting dilution in Vero CCL-81 cell culture and the plaque assay with the same cell cultures.
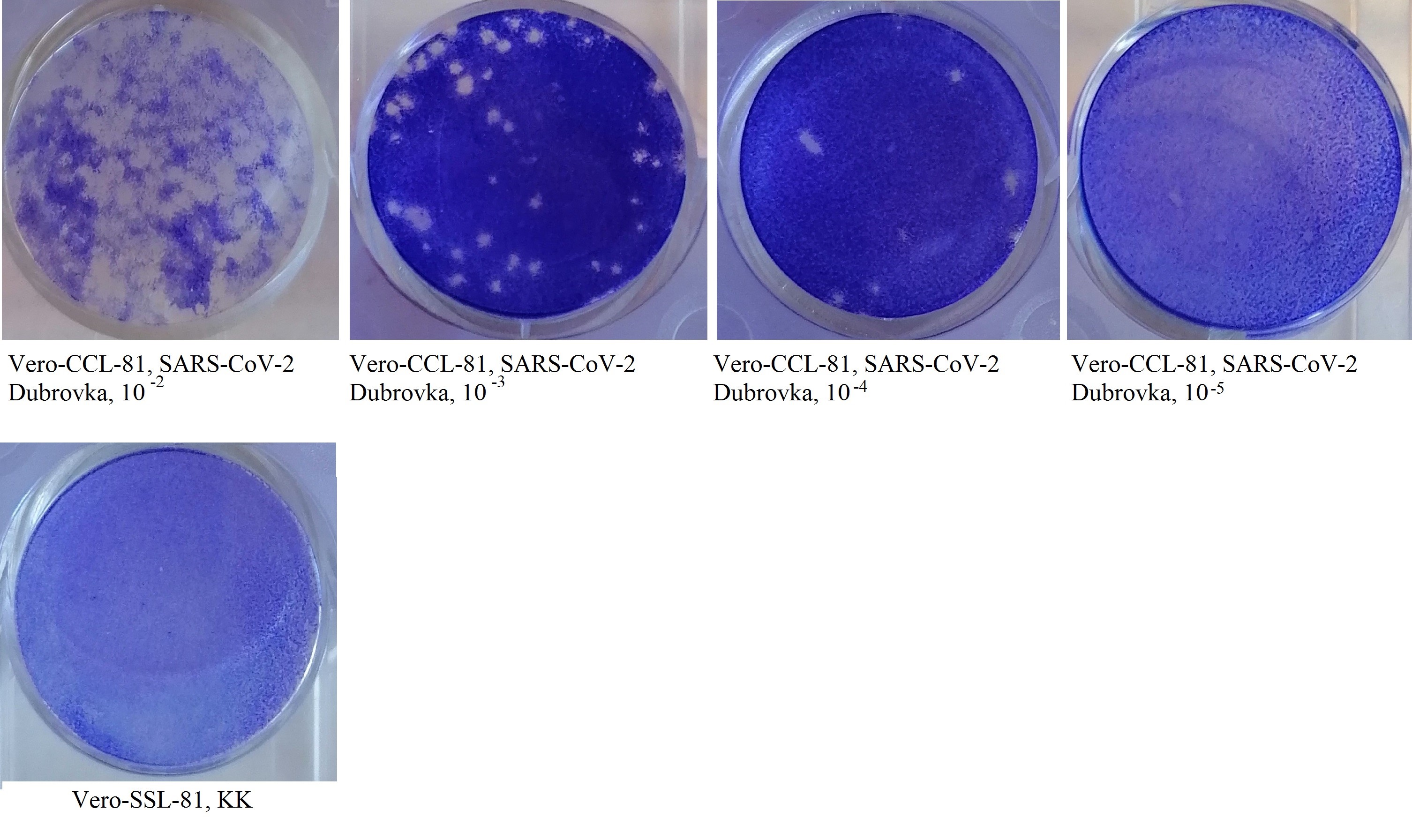
Based on CPE, the SARS-CoV-2 titer was 4.50 lg TCD50/0.2 ml; based on the plaque assay, it was 4.55 PFU50/0.2 ml. The VRI test was performed using 10 doses of virus; the virus titer was 3.5 lg TCD50/0.2 ml or 3.5 lg PFU50/0.2 ml (Fig. 1).
Plaque assay in the Vero CCL-81 cell monolayer infected with SARS-CoV-2 Dubrovka.
When interacting with 10 doses of SARS-CoV-2 Dubrovka, ACOPB had virus-inhibitory activity at 1 : 32 dilution, demonstrating 100% protection of cells during 8 days of culturing (the monitoring period).
To confirm the virus-inhibitory activity of ACOPB against SARS-CoV-2 Dubrovka, we conducted tests aimed to measure expression levels of RIFN-α/β and -γ on membranes of human PBMCs. At the same time, this method was used to identify the genesis of the protective activity of bacterial antigens present in ACOPB. In these tests, mouse monoclonal anti-idiotypic antibodies mimicking biological properties of human IFN-α/β and -γ, i.e. anti-receptor antibodies were used as a highly specific marker.
Earlier, we found that when PBMCs were induced in vitro by ACOPB, the expression of RIFN-α/β and -γ started more effectively at medication dilution of 1:10 or at 10 µg of the medication. Therefore, we decided to find the optimum dose of ACOPB, which would induce in vitro the highest expression of IFN-R on PBMC membranes.
Table 2 shows expression levels of RIFN-α/β on human PBMCs, which were induced by different dilutions of the medication as well as by the mixture of ACOPB with 10 doses of SARS-CoV-2, after they interacted for 2 hours at +4ºC prior to being dispensed into cultured lymphocytes.
Table 2. Expression of RIFN-α/β (%) in human PBMCs induced in vitro by ACOPB and ACOPB with SARS-CoV-2 Dubrovka strain, hours
Induction time, hours | ACOPB dilution (dose) | Control (mean values) RINF-α | |||||||||
1 : 10 (10 мкг | µg) | decrease, % | 1 : 20 (5 мкг | µg) | decrease, % | 1 : 40 (2,5 µg) | decrease, % | ||||||
ACOPB | ACOPB + SARS-CoV-2 | ACOPB | ACOPB + SARS-CoV-2 | ACOPB | ACOPB + SARS-CoV-2 | human peripheral blood mononuclear cells | SARS-CoV-2 | ||||
1 | 0.7 ± 0.001 | 0.4 ± 0.02 | 0.3* | 0.5 ± 0.04 | 0.3 ± 0.01 | 0.2* | 0.5 ± 0.03 | 0.2 ± 0.07 | 0.3* | 0.60 ± 0.03 | 0.60 ± 0.05 |
6 | 3.1 ± 0.05 | 2.6 ± 0.01 | 0.5* | 4.1 ± 0.09 | 2.4 ± 0.04 | 1.7* | 2.8 ± 0.1 | 2.0 ± 0.04 | 0.8* | ||
24 | 5.3 ± 0.07 | 3.8 ± 0.04 | 1.5* | 7.8 ± 0.08 | 6.0 ± 0.07 | 1.8* | 7.3 ± 0.01 | 5.0 ± 0.09 | 2.3* | ||
30 | 6.0 ± 0.09 | 5.0 ± 0.07 | 1.0* | 10.0 ± 0.05 | 6.0 ± 0.05 | 4.0* | 6.5 ± 0.04 | 5.0 ± 0.03 | 1.5* | ||
44 | 3.5 ± 0.01 | 2.5 ± 0.09 | 1.0* | 8.0 ± 0.04 | 5.5 ± 0.07 | 2.5* | 3.0 ± 0.03 | 2.5 ± 0.05 | 0.5* | ||
48 | 3.0 ± 0.08 | 2.0 ± 0.04 | 1.0* | 5.0 ± 0.02 | 3.0 ± 0.04 | 2.0* | 3.0 ± 0.05 | 2.0 ± 0.02 | 1.0* | ||
50 | 2.5 ± 0.01 | 2.0 ± 0.06 | 0.5* | 4.5 ± 0.02 | 3.0 ± 0.03 | 1.5* | 3.0 ± 0.05 | 1.5 ± 0.03 | 1.5* | ||
Note. *р ≤ 0,05.
The analysis of the expression of RIFN-α/β induced on lymphocyte membranes by ACOPB shows (Table 2) that the most effective induction with all dilutions of the medication starts 6 hours after its beginning and reaches the highest level 24–30 after its beginning, and then its level gradually decreases. It should be noted that all doses of the medication cause in vitro RIFN-α/β induction on lymphocyte membranes, i.e. the synthesis of human IFN-α/β. Note that the maximum synthesis of IFN-α/β in vitro is reached at medication dilution of 1:20, i.e. at 5 µg of the medication.
The expression of RIFN-α/β induced in vitro on lymphocyte membranes using the ACOPB and SARS-CoV-2 Dubrovka mixture starts decreasing 6 hours after the induction and continues throughout the study period (Table 2). The lowest expression level of RIFN-α/β is reached 30 hours after the induction; the most effective decrease in the expression level is observed when lymphocytes are induced with the ACOPB and coronavirus mixture at 1:20 dilution or 5 µg (p ≤ 0.05). The obtained results mean that ACOPB inhibits replication SARS-CoV-2 Dubrovka, neutralizing its infectivity. This conclusion was supported by the results of the VRI test performed with Vero CCL-81 cell culture susceptible to SARS-CoV-2 Dubrovka.
The above results clearly demonstrate that ACOPB is an effective immunomodulatory medication that also has a virus-inhibitory effect. This conclusion is confirmed by the data on the levels of RIFN-γ (Table 3). The expression level of RIFN-γ, i.e. the synthesis of immune IFN by lymphocytes induced in vitro by ACOPB and by the mixture of the medication with SARS-CoV-2 Dubrovka involved the same mechanisms as the induction of RIFN-α/β. The analysis of the data presented in Table 3 shows that ACOPB used in the specified amounts can induce in vitro RIFN-γ expression on membranes of lymphocytes cultured in vitro 6 hours after the beginning of the induction, with the duration lasting up to 50 hours (the monitoring period). Active expression of RIFN-γ is observed from 24 hours to 44 hours from the induction by ACOPB; the highest induction is reached at concentrations of 10 and 5 µg. The expression of RIFN-γ decreases when lymphocytes are induced by ACOPB after it has interacted with SAPS-CoV-2 Dubrovka for 2 hours, thus confirming virus-inhibitory activity of ACOPB.
Table 3. Expression of RIFN-γ (%) in human PBMCs induced in vitro by ACOPB and the ACOPB and SARS-CoV-2 Dubrovka strain mixture, hours
Induction time, hours | Разведение КАУПБ (доза) | ACOPB dilution (dose) | Control (mean values) RINF-α | |||||||||
1 : 10 (10 µg) | decrease, % | 1 : 20 (5 µg) | decrease, % | 1 : 40 (2,5 µg) | decrease, % | ||||||
ACOPB | ACOPB + SARS-CoV-2 | ACOPB | ACOPB + SARS-CoV-2 | ACOPB | ACOPB + SARS-CoV-2 | human peripheral blood mononuclear cells | SARS-CoV-2 | ||||
1 | 0.6 ± 0.07 | 0.6 ± 0.05 | 0 | 0.6 ± 0.04 | 0.8 ± 0.03 | 0 | 0.7 ± 0.02 | 0.6 ± 0.05 | 0.1* | 0.57 ± 0.03 | 0. 55 ± 0.03 |
6 | 2.4 ± 0.01 | 2.4 ± 0.09 | 0 | 3.8 ± 0.05 | 3.2 ± 0.05 | 0.6* | 3.4 ± 0.01 | 3.0 ± 0.07 | 0.4* | ||
24 | 4.5 ± 0.03 | 3.5 ± 0.01 | 1.0* | 5.5 ± 0.02 | 4.5 ± 0.06 | 1.0* | 4.8 ± 0.04 | 3.8 ± 0.03 | 1.0* | ||
30 | 6.5 ± 0.01 | 3.5 ± 0.09 | 3.0* | 7.5 ± 0.05 | 3.5 ± 0.05 | 4.0* | 4.0 ± 0.07 | 3.0 ± 0.04 | 1.0* | ||
44 | 4.5 ± 0.02 | 3.0 ± 0.03 | 1.0* | 5.0 ± 0.01 | 3.5 ± 0.05 | 1.5* | 4.0 ± 0.06 | 3.0 ± 0.01 | 1.0* | ||
48 | 3.5 ± 0.03 | 2.5 ± 0.02 | 1.0* | 4.0 ± 0.07 | 2.5 ± 0.07 | 1.5* | 3.5 ± 0.01 | 2.5 ± 0.05 | 1.0* | ||
50 | 3.0 ± 0.05 | 2.5 ± 0.09 | 0.5* | 3.5 ± 0.04 | 2.5 ± 0.01 | 1.0* | 3.0 ± 0.07 | 2.0 ± 0.06 | 1.0* | ||
Note. *р ≤ 0,05.
Discussion
ACOPB is used for effective prevention and treatment of most of the chronic upper and lower respiratory tract diseases. It has been found that ACOPB has a protective effect against viral infections — influenza and herpes virus infections. The COVID-19 pandemic triggered the need to find out whether this medication had a protective effect when administered for prevention and treatment of human coronavirus infection. For this purpose, we used the Russian strain of SARS-CoV-2 — Dubrovka isolated from a patient with COVID-19 and adapted to the Vero CCL-81 cell culture.
HA performed for Vero CCL-81 cell culture infected with SARS-CoV-2 Dubrovka strain detected a high titer of hemagglutinin, which is a target for antiviral agents, reaching over 1:256, and its low content in VCF.
To perform the VRI test with ACOPB, the exact titer of the virus must be determined. SARS-CoV-2 was titrated using two methods: the limiting dilution in Vero CCL-81 cell culture and the plaque assay with the same cell culture. The virus-inhibitory titer of ACOPB with 10 doses of SARS-CoV-2 was 1:32, demonstrating 100% protection of cells for 8 days (the monitoring period).
It was also important to find out what caused the protective effect of ACOPB. It is known that IFNs are required for implementation of the immune response to an antigenic stimulus, and that any antigen is an interferonogen [10]. Previously, we, using mouse monoclonal anti-idiotypic antibodies structurally mimicking human IFN-α/β and -γ, demonstrated that the infection-associated activation of the immune system was represented by expression of RIFN-α/β and -γ in immunocompetent human cells [12, 13]. The indirect membrane immunofluorescence assay showed that when delivered in vitro into cultured human lymphocytes, ACOPB induced RIFN-α/β and -γ, thus demonstrating its strong immunomodulatory effect.
When ACOPB interacts with 10 doses of SARS-CoV-2 Dubrovka strain for at least 2 hours and then is delivered into lymphocytes cultured in vitro, the expression level of RIFN-α/β and -γ decreases. These findings suggest that ACOPB has a virus-inhibitory effect, and its protective effect is provided by endogenous IFN-α/β and -γ synthesized in the body.
About the authors
Oksana A. Svitich
I. Mechnikov Research Institute of Vaccines and Sera
Email: svitich_o_a@staff.sechenov.ru
ORCID iD: 0000-0003-1757-8389
D. Sci. (Med.), Prof., Corresponding Member of RAS, Head, Department of immunology and allergology, Director
Russian Federation, MoscowFiraya G. Nagieva
I. Mechnikov Research Institute of Vaccines and Sera
Author for correspondence.
Email: fgn42@yandex.ru
ORCID iD: 0000-0001-8204-4899
D. Sci. (Med.), Assoc. Prof., Head, Laboratory of hybrid cell cultures, Department of virology
Russian Federation, MoscowEkaterina A. Kurbatova
I. Mechnikov Research Institute of Vaccines and Sera
Email: kurbatova6162@yandex.ru
ORCID iD: 0000-0002-4474-7531
D. Sci. (Med). Prof., Head, Laboratory of therapeutic vaccine
Russian Federation, MoscowElena P. Barkova
I. Mechnikov Research Institute of Vaccines and Sera
Email: e.barkova2012@yandex.ru
ORCID iD: 0000-0002-3369-8869
Cand. Sci. (Biol.), leading researcher, Laboratory of hybrid cell cultures, Department of virology
Russian Federation, MoscowOlga S. Kharchenko
I. Mechnikov Research Institute of Vaccines and Sera
Email: bio139@yandex.ru
ORCID iD: 0000-0002-2169-9610
researcher, Laboratory of DNA viruses, Department of virology
Russian Federation, MoscowAleksandra D. Stroeva
I. Mechnikov Research Institute of Vaccines and Sera
Email: aleksandra.26@mail.ru
ORCID iD: 0000-0002-4179-931X
junior researcher, Laboratory of hybrid cell cultures, Department of virology
Russian Federation, MoscowEvgeny A. Pashkov
I. Mechnikov Research Institute of Vaccines and Sera
Email: svitich_o_a@staff.sechenov.ru
ORCID iD: 0000-0002-5682-4581
junior researcher, Laboratory of molecular immunology, Department of immunology and allergology
Russian Federation, MoscowAlexey N. Lisakov
I. Mechnikov Research Institute of Vaccines and Sera
Email: lisakov@mail.ru
ORCID iD: 0000-0001-9374-5842
researcher, Laboratory of hybrid cell cultures, Department of virology
Russian Federation, MoscowAnastasiia V. Gracheva
I. Mechnikov Research Institute of Vaccines and Sera
Email: gr54@yandex.ru
ORCID iD: 0000-0001-8428-4482
junior research, Laboratory of molecular virology
Russian Federation, MoscowMariia B. Potapova
I.M. Sechenov First Moscow State Medical University (Sechenov University)
Email: svitich_o_a@staff.sechenov.ru
ORCID iD: 0000-0001-9647-1322
postgraduate student, Department of skin and venereal diseases named after V.A. Rakhmanov
Russian Federation, MoscowEvgeny B. Faizuloev
I. Mechnikov Research Institute of Vaccines and Sera
Email: feb@mail.ru
ORCID iD: 0000-0001-7385-5083
Cand. Sci. (Biol.), Head, Laboratory of molecular virology
Russian Federation, MoscowVitaly V. Zverev
I. Mechnikov Research Institute of Vaccines and Sera
Email: vitalyzverev@outlook.com
ORCID iD: 0000-0001-5808-2246
D. Sci. (Biol.), Prof., Academician of RAS, Head, Laboratory of molecular biotechnology
Russian Federation, MoscowReferences
- Akhmatova N.K. Molecular and cellular mechanisms of action of immunomodulators of microbial origin on the functional activity of the effectors of innate immunity: Diss. Moscow; 2006.
- Pashenkov M.V., Pinegln B.V. Cell physiology of innate immune system: dendritic cells. Immunology. 2006;27(6):368–78. EDN: https://www.elibrary.ru/hykkzd
- Egorova N.B., Kurbatova E.A., Akhmatova N.K., Semenova I.B. Protective activity of immunovacvp-4 vaccine against avian influenza virus H5N2 administered by different methods. Journal of Microbiology, Epidemiology and Immunobiology. 2011;88(1):49–53. EDN: https://www.elibrary.ru/qbbzsx
- Egorova N.B., Kurbatova E.A., Semenova I.B. Vaccines and Vaccination: National Guidelines. Moscow; 2011:693–714.
- Glad'ko O.V., Egorova N.B., Masyutova S.A., et al. Immunotherapy of genital herpes with a multicomponent VP-4 vaccine. Military Medical Journal. 2002;323(5):73–6.
- Chuchalin A.G., Osipova G.L., Egorova N.B., et al. Controlled studies on the effectiveness of a multicomponent vaccine in immunotherapy in patients with chronic obstructive respiratory diseases. Russian Pulmonology. 1995;(2):55–61. EDN: https://www.elibrary.ru/xctiqb
- Nemykina O.E., Egorova N.B., Shcherbakova B.V., et al. Optimization of treatment of atopic dermatitis with the help of immunotherapy. Journal of Microbiology, Epidemiology and Immunobiology. 2005;85(4):53–7. EDN: https://www.elibrary.ru/ymzeiw
- Antonova L.P., Markova T.P., Kurbatova E.A. Application of polycomponent vaccine VP-4 by combined nasal-subcutaneous method in the treatment of patients with bronchial asthma and chronic obstructive bronchitis. Journal of Microbiology, Epidemiology and Immunobiology. 2004;84(6):36–40.
- Nemykina O.E., Egorova N.B., Shcherbakova B.V., et al. Immunological characteristics in the therapy of atopic dermatitis in children with polycomponent vaccine Immunovac ВП-4. Journal of Microbiology, Epidemiology and Immunobiology. 2005;85(5):45–9. EDN: https://www.elibrary.ru/hsuwwp
- Hu B., Guo H., Zhou P., Shi Z.L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021;19(3):141–54. DOI: https://doi.org/10.1038/s41579-020-00459-7
- Harrison A.G., Lin T., Wang P. Mechanisms of SARS-CoV-2 transmission and pathogenesis. Trends Immunol. 2020;41(12): 1100–5. DOI: https://doi.org/10.1016/j.it.2020.10.004
- Tu Y.F., Chien C.S., Yarmishyn A.A., et al. A review of SARS — CoV-2 and the ongoing clinical trials. Int. J. Mol. Sci. 2020;21(7):2657. DOI: https://doi.org/10.3390/ijms21072657
- Gracheva A.V., Korchevaya E.R., Kudryashova A.M., et al. Adaptation of the MTT assay for detection of neutralizing antibodies against the SARS-CoV-2 virus. Journal of Microbiology, Epidemiology and Immunobiology. 2021;98(3):253–65. DOI: https://doi.org/10.36233/0372-9311-136 EDN: https://www.elibrary.ru/jglovv
- Barkova E.P., Nagieva F.G., Kuznetsov V.P., et al. Expression of receptors for human interferons alpha and gamma on the surface of peripheral blood mononuclear cells in some viral infections. Problems of Virology. 1998;43(6):16–8. EDN: https://www.elibrary.ru/wiapnb
- Lisakov A.N., Nagieva F.G., Barkova E.P., et al. The immunocompetent cells receptors research under experimental influenza infection in vitro. Russian Journal of Infection and Immunity. 2015;5(3):273–8. DOI: https://doi.org/10.15789/2220-7619-2015-3-273-278 EDN: https://www.elibrary.ru/ukjpgj
- Shubladze A.K., Gaidamovich S.Ya. A Short Course of Practical Virology. Moscow;1954:92–3.
- Mikhaylova N.A., Nagieva F.G., Grinko O.M., Zverev V.V. Experimental study of antiviral activity of spore-forming bacterium Bacillus pumilus "Pashkov". Journal of Microbiology, Epidemiology and Immunobiology. 2010;87(2): 69–74. EDN: https://www.elibrary.ru/rurigl
- Bracci N., Pan H.C., Lehman C., et al. Improved plaque assay for human coronaviruses 229 E and OC43. PeerJ. 2020;8:e10639. DOI: https://doi.org/10.7717/peerj.10639
- Norrby E. Hemagglutination by measles virus. 4. A simple procedure for production of high potency antigen for hemagglutination-inhibition (HI) tests. Proc. Soc. Exp. Biol. Med. 1962; 111:814–8. DOI: https://doi.org/10.3181/00379727-111-27930
Supplementary files