Possibilities and prospects of using biofluorescent proteins at the stage of preclinical evaluation of live vaccines, using the example of the Yersinia pestis vaccine strain EV NIIEG pTURBOGFP-B
- Authors: Klyueva S.N.1, Budanova A.A.1, Kravtsov A.L.1, Bugorkova S.A.1
-
Affiliations:
- Russian Anti-Plague Institute "Microbe"
- Issue: Vol 102, No 2 (2025)
- Pages: 190-200
- Section: ORIGINAL RESEARCHES
- URL: https://microbiol.crie.ru/jour/article/view/18827
- DOI: https://doi.org/10.36233/0372-9311-627
- EDN: https://elibrary.ru/IGXJFZ
- ID: 18827
Cite item
Abstract
Introduction. Currently, studies aimed at finding the most informative and optimized method for assessing the survival rate of the plague microbe vaccine strain in the body of animals vaccinated against plague are relevant.
Aim — to evaluate the feasibility of using biofluorescent proteins using the example of the Yersinia pestis vaccine strain EV NIIEG pTurboGFP-B (EVGFP) in combination regimens with immunomodulators at the stage of preclinical evaluation of live vaccines.
Materials and methods. Guinea pigs were immunized with EVGFP grown at 28ºC and 37ºC (EVGFP28 and EVGFP37, respectively), in combination with immunomodulators (azoximer bromide, AB, and human recombinant interferon gamma, HRI).
Results. Fluorescence microscopy revealed seeding (up to 600 m.c. in one field of view) with EVGFP cells at the site of culture introduction in all experimental groups on the 1st day. In vivo flow cytometry showed that on the 1st day in all experimental groups the phagocytic index (PI) averaged 94.5%, with a subsequent decrease by the 4th day by an average of 4.4 times (21.2%). On the 4th day of the study in the EVGFP37+AB group the PI exceeded the similar indicator in the EVGFP37 group by 1.8 times. On the contrary, in the EVGFP28+HRI group the PI decreased by 2.2 times relative to the similar indicator in the EVGFP28 group. In addition, in the EVGFP37+AB and EVGFP37+HRI groups, on day 4, the PI was 2 times higher than in the EVGFP28+AB and EVGFP28+HRI groups, respectively. In the EVGFP37 group, the phagocytic number was on average 1.5 times higher than in the EVGFP28 group.
Conclusion. The obtained data confirm the dependence of the outcome of in vivo interaction of the plague microbe with spleen phagocytes on the temperature of bacterial growth, as well as on the presence of AB and HRI. The use of biofluorescent proteins, as shown by the example of the EVGFP strain and the flow cytometry method, expands the possibilities for assessing live plague vaccines in preclinical studies.
Full Text
Introduction
In recent years, various fluorescent proteins have been used as easily detectable markers of microorganisms in biological and medical research. One of such proteins is the green fluorescent protein GFP (green fluorescent protein) found in the jellyfish Aequorea victoria [1, 2]. The advantages of using GFP protein compared to other reporter proteins are its ability to fluoresce in the absence of any cofactor or substrate, prolonged signal, low metabolic toxicity, and absence of background fluorescence. To date, a wide variety of different plasmids engineered with GFP are available and have been successfully used. For example, the commercial vector pTurboGFP-B provides stable expression and rapid maturation of fluorescent protein [2].
Engineered strains of Y. pestis producing GFP are used to study the conditions of symbiosis formation with protozoa and/or modeling of interaction with host cells (mammals — rodents) [3, 4], with a vector (fleas) [5]. The fluorescent protein GFP as a biosensor has been successfully used to detect Y. pestis in mixed cultures, tracking bacteria in vitro and in vivo, establishing intracellular localization of cells of recombinant strains of Y. pestis, assessing phagocytosis of Y. pestis by macrophages of BALB/c mice [6–9]. Genomic technologies have made it possible to use GFP as a molecular vector for the development of vaccines against various bacterial and viral infections of humans and animals [1, 10].
One of the main tasks of preclinical studies in the development of live vaccines against plague is to determine the degree of residual virulence (harmlessness) of the vaccine strain of the plague microbe in terms of engraftment and spread in the macroorganism. Traditionally, live cell engraftment of plague microbe strains has been recorded using the bacteriological method. Labeling of strains of Y. pestis strains with fluorescent proteins opens new possibilities that allow in vivo monitoring microorganisms using a number of other techniques, including luminescence microscopy, which provides visualization of the plague pathogen by the presence of a specific fluorescent glow [3, 4], and flow cytometry, which helps to determine the number of live microbial cells by light scattering and fluorescence intensity of each individual cell in a suspension of organs [11].
It is known that the reference Y. pestis vaccine strain EV NIIEG takes root and reproduces in the organs of laboratory animals, which contributes to the development of active plague immunity [12]. One of the most significant factors influencing the engraftment of the plague pathogen, which is able to multiply in various conditions similar to its habitat in the bodies of warm-blooded mammals (37°C) and poikilothermic fleas (20–28°C), is temperature [13]. The temperature-dependent adaptation strategy of Y. pestis is an essential part of the concept of the bacterium overcoming innate immunologic defense mechanisms, such as phagocytosis, and the induction of an inflammatory response by macrophages and neutrophils [13].
The use of various immunomodulators in the scheme of plague vaccination allows to reduce the antigenic load on the body without reducing the intensity of the immune response. Thus, azoxymer bromide (AB) in combination with the Y. pestis vaccine strain EV NIIEG has a stimulating effect on the reactivity of cells of the phagocytic system of laboratory animals, increases the protective activity of live plague vaccine almost 3 times and, as well as human recombinant interferon-γ (HRI), stimulates antibody formation and cytokine response [14–16].
Taking into account all of the above facts, an attempt was made to expand the possibility of assessing the effectiveness and duration of the non-sterile phase of the immune response, which is an obligatory stage in the formation of specific plague immunity, through the use of fluorescent proteins in testing various schemes of live plague vaccine administration.
The aim of the study is to evaluate the feasibility of using biofluorescent proteins on the example of the Y. pestis vaccine strain EV NIIEGP pTurboGFP-B in schemes of its combined use with immunomodulators at the stage of preclinical evaluation of live vaccines.
Materials and methods
To create a GFP-producing strain, the Y. pestis vaccine strain EV NIIEG was used. The gene encoding TurboGFP synthesis was introduced as part of the commercial vector plasmid pTurboGFP-B (4103 bp, “Evrogen”) by electroporation according to the recommendations [17]. Electroporation was performed on a Gene Pulser Xcell device (“Bio-Rad”) using a standard protocol for prokaryotic cells. The presence of commercial plasmid was determined by antibiotic resistance marker by seeding the strain on LB agar plates with 50 μg/mL ampicillin. Colonies were viewed with the naked eye, as well as on a “Axio Lab.A1” fluorescent microscope (“Carl Zeiss Microscopy GmbH”), registering intense fluorescent glow in the ultraviolet region of the spectrum. The constructed recombinant strain was designated Y. pestis EV NIIEG pTurboGFP-B (EVGFP) and was deposited under the number KM 2115 in the State Collection of Pathogenic Bacteria of the Russian Anti-Plague Institute “Microbe” of Rospotrebnadzor.
The Y. pestis strain EV NIIEG was grown on LB agar (pH 7.2), and the biofluorescent strain EVGFP was grown on LB agar (pH 7.2) with ampicillin (50 mg/mL) for 48 h at 28°C. Furthermore, EVGFP cell culture with increased resistance to leukocyte phagocytosis was used [18]. For this purpose, EVGFP cells were seeded from a 2-day 28°C culture at a final concentration of 1 × 107 CFU/mL on LB broth (pH 7.2) and cultured under aeration conditions at 37°C for 18 h. Suspensions were prepared from EVGFP cultures grown at 28°C (EVGFP28) and 37°C (EVGFP37) using the turbidity standard CCA 42-28-59-85P at a concentration of 4 × 109 CFU/mL.
The experimental model was guinea pigs weighing 250-350 g obtained from the Experimental animals department with a vivarium of the Russian Anti-Plague Institute “Microbe”. The animals were divided into 6 experimental groups of 12 animals each. Guinea pigs were subcutaneously immunized with the EVGFP strain grown at 28°C (groups 1–3) and 37°C (groups 4–6) at a dose of 2 × 109 CFU/0.5 mL. Guinea pigs from groups 2 and 5 were additionally subcutaneously injected with AB (“PetrovaxPharm”) at a concentration of 60 μg (EVGFP28+AB and EVGFP37+AB, respectively) 1 h before immunization. Biomodels of groups 3 and 6 additionally received HRI (“Pharmaclone”) at a concentration of 2000 IU (EVGFP28+HRI and EVGFP37+HRI, respectively). The control group 7 consisted of intact guinea pigs (4 individuals). All manipulations with animals were carried out in accordance with the legislation of the Russian Federation and international principles. Animal immunization experiments were performed in accordance with Sanitary Rules and Standards 3.3686-21 “Sanitary and Epidemiological Requirements for the Prevention of Infectious Diseases”. The program of experimental work with animals was approved by the Bioethics Commission of the Russian Anti-Plague Institute “Microbe” (Protocol No. 5 of 25.05.2023).
The biochemical properties of Y. pestis was studied using API standard biochemical test strips (“bioMérieux SA”) according to the manufacturer’s instructions.
Morphology of bacterial cells was evaluated using an Olympus CX41light microscope (“Olympus”) and a VZ-C31S digital camera (“VideoZavr”) in the VideoZavr v. 1.5 program at magnifications of 40 and 100.
The engraftment of EVGFP strain in guinea pig organs was evaluated by microscopic and flow cytometric methods. On the 1st, 4th, 7th and 14th days of immunogenesis, animals were sacrificed using chloroform, dissected and smears of internal organs (injection site, inguinal lymph nodes, blood, spleen, liver, lungs) were taken. The smears-imprints of animal organs were viewed in an Axio LAB.A1fluorescent microscope (“Carl Zeiss”) with A-Plan 100x/1.25 OiI objective lens at a magnification of × 1000. The specimens were examined under the microscope and photographed at 5 fields of view per preparation. Photographs were taken using an AxioCam ERc5s camera (“Carl Zeiss”).
To investigate the engraftment of Y. pestis EV NIIEG pTurboGFP using flow cytometry, a suspension of spleen cells at a concentration of 106 cells/mL was prepared in RPMI-1640 medium with gentamicin (100 μg/mL) using the standard method. Then to 100 μL of the obtained suspension was added 1 mL of BD FACS Lysing Solution (“BD Biosciences”) diluted 10 times (according to the instructions) for lysis of erythrocytes and fixation of leukocytes and samples were incubated for 20 min.
Cell suspensions were analyzed on a СyAn ADP flow cytofluorimeter in the Summit v.4.3 Built 2445 program. Detection of EVGFP bacteria in phagocytes (macrophages and neutrophils) of guinea pig spleen was performed according to the previously developed protocol for determination of phagocytic reaction indices in human blood and animals with FITC-labeled Y. pestis EV NIIEG cells [15, 19]. In spleen cell suspensions, phagocytes were differentiated by light scattering parameters (size and degree of granularity) from lymphocytes (Fig. 3, a), and then by gating the phagocytic population the percentage of fluorescent phagocytes (macrophages, neutrophils) was determined in the spleen, which corresponded to the relative content of active phagocytes (PI — phagocytic index, %) that absorbed in vivo live cells of the tested biofluorescent strain of the plague microbe. The average number of bacteria absorbed by phagocytes (PN — phagocytic number) was estimated by the average value of their luminescence intensity in the green region of the spectrum (Mean), measured in conventional units of fluorescence intensity (cytofluorimeter channels) [14, 19–21].
Statistical processing of the obtained results was performed using the Microsoft Office Excel 2016, Statistica 10.0 (“StatSoft Inc.”) standard software package. The data were presented as median (Me) and quartile deviations (Q25; Q75) with calculation of reliability of differences in the studied groups using Mann–Whitney U-criterion.
Results
Comparative culture analysis of the original vaccine strain and biofluorescently labeled vaccine strain
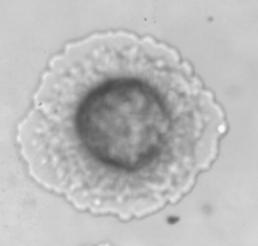
The culture, morphological and biochemical properties of recombinant EVGFP and the original Y. pestis EV NIIEG strains were compared. It was found that the recombinant strain had cell morphology typical of the plague pathogen. Cells of the strain EVGFP carrying the GFP fluorescent protein gene were identified by the presence of green fluorescent glow of the bacteria. On LB agar with ampicillin, strain EVGFP formed characteristic R-type colonies of yellow-green color (Fig. 1).
Fig. 1. R-type of colonies of Y. pestis strain EV NIIEG pTurboGFP-B, ×40 (а) and ×100 (b).
The characteristic features of the growth of the plague pathogen in liquid nutrient medium were a clear broth and a loose, powdery or flake-like sediment at the bottom of the test tube, which easily disintegrated when shaken. Based on the analysis of biochemical properties, it was found that the recombinant strain EVGFP did not differ in its characteristics from the original Y. pestis strain EV NIIEG. Both strains fermented glucose, mannitol, arabinose, and did not degrade inositol, sorbitol, rhamnose, sucrose, melibiose and amygdalin.
Administration of the EVGFP strain to guinea pigs at a massive dose of 2 × 109 CFU did not cause death of the biomodels during the entire observation period.
Thus, the studied EVGFP strain did not differ from the original Y. pestis strain EV NIIEG in its cultural, morphological and biochemical properties, and also corresponded to the reference vaccine strain in terms of harmlessness.
Evaluation of the engraftment of Y. pestis strain EV NIIEG pTurboGFP by luminescence microscopy
During microscopic examination, EVGFP cells were detected in smear-prints only from the site of culture administration in all groups of immunized guinea pigs and only on the 1st day of immune response (Fig. 2).
Fig. 2. Detection of cells of the biofluorescent Y. pestis vaccine strain EV NIIEG pTurboGFP-B in imprint smears of the subcutaneous tissue of the guinea pig thigh (injection site) on day 1 of the immune response at ×1000 magnification. а — image in the microscope eyepiece; b — computer monitor image.
Cells of the fluorescent strain were visualized as bright green sticks. The number of bacteria was 400 ± 100 m bacteria in one field of view, indicating abundant EVGFP cell infiltration of the injection site. On further observation on the 4th, 7th and 14th days of immunogenesis, no cells of the recombinant strain were registered in the smear-prints of all examined organs of guinea pigs.
Evaluation of the engraftment of Y. pestis strain EV NIIEG pTurboGFP using flow cytofluorimetric technology
Taking into account the fact that spleen neutrophils and macrophages are one of the main objects for assessing phagocytosis and engraftment of Y. pestis [11], it was reasonable to use guinea pig spleen cells for cytometric studies.
Fig. 3. Fluorescence intensity of phagocytes of the spleen of guinea pigs immunized with the biofluorescent Y. pestis vaccine strain EV NIIEG pTurboGFP-B (37°С) in the dynamics of the immune response.
Cytogram а: area R1 corresponds to the total number of phagocytes FS/SS dot plot of a sample of guinea pig spleen cells inoculated with the original Y. pestis vaccine strain EV NIIEG (control). The characteristic distribution of individual spleen phagocytes by size (FS) and degree of granularity (SS) is presented. Spleen phagocytes (28.91% of cells) are localized in the R1 region of the cytogram.
Active phagocytes are localized in the histograms in the R4 region: b–e — days 1, 4, 7 and 14 respectively, after immunization of guinea pigs with the Y. pestis EV NIIEG pTurboGFP-B (37°С).
The intensity of the fluorescence signal of GFP protein was used to determine the presence of EVGFP in the population of spleen phagocytes (macrophages and neutrophils), and the indices of the in vivo phagocytic reaction were taken into account. The histograms in Fig. 3, b–d demonstrate the dynamics of the decrease in the relative number of phagocytes in the spleen characterized by intense green fluorescence due to the uptake of cells of EVGFP strain grown at 37°C.
Fig. 3 clearly shows that in the interval from 1 to 4 days the proportion of fluorescent phagocytes decreased from 94.54 to 21.23%, and by the 14th day — to 0, i.e. to the values characteristic of spleen phagocytes of intact (control) animals, which do not have fluorescent luminescence in the green region of the spectrum (Fig. 3, e).
Comparative evaluation of the effect of immunomodulatory drugs in combined use with biofluorescent strain and conditions of its cultivation on phagocytic activity of spleen cells
At the next stage, we analyzed the efficiency of drug application on the outcome of interaction of the studied EVGFP strain with guinea pig spleen phagocytes under in vivo conditions. On the 4th day of immunogenesis, a significant decrease in PI in the EVGFP28+ HRI group was found compared to the same index in the EVGFP28 group (Table).
Detection of the biofluorescent Y. pestis vaccine strain EV NIIEG pTurboGFP in guinea pig spleen phagocytes during immunization in combination with immunomodulators according to flow cytometry data, Me (Q25; Q75)
Group | Immunization | Day | Phagocytic | Phagocytic |
1 | EVGFP28 | 1 | 89.2 (83.0; 95.4) | 19.3 (17.0; 21.5) |
4 | 19.8 (16.6; 22.0) | 12.6 (11.8; 13.4) | ||
7 | 0.07 (0; 0.1) | 1.6 (0.9; 2.3) | ||
14 | 0 | 0.7 (0.5; 0.8) | ||
2 | EVGFP28+AB | 1 | 99.1 (98.0; 99.4) | 24.8 (20.7; 28.9) |
4 | 17.5 (15.4; 19.6) | 19.2 (17.5; 20.9)* | ||
7 | 0.02 (0; 0.05) | 10.0 (8.9; 11.2)* | ||
14 | 0 | 0 | ||
3 | EVGFP28+HRI | 1 | 97.4 (95.5; 99.4) | 22.1 (18.0; 26.2) |
4 | 9.0 (8.4; 9.6)* | 18.2 (15.7; 20.8) | ||
7 | 0.06 (0; 0.1) | 8.7 (7.9; 9.5)* | ||
14 | 0 | 1.5 (1.3; 1.7) | ||
4 | EVGFP37 | 1 | 92.5 (87.8; 97.2) | 19.6 (16.2; 23.0) |
4 | 21.2 (18.4; 24.0) | 20.1 (15.4; 24.8)# | ||
7 | 0.1 (0.05; 0.20) | 10.0 (8.3; 11.7) | ||
14 | 0.1 (0.05; 0.20) | 1.0 (0.9; 1.1) | ||
5 | EVGFP37+AB | 1 | 98.5 (96.8; 99.2) | 25.2 (20.0; 30.4) |
4 | 37.1 (37.0; 41.2)*# | 17.5 (14.4; 20.6) | ||
7 | 0.2 (0.1; 0.3) | 10.7 (8.1; 13.3) | ||
14 | 0 | 0.3 (0.1; 0.5) | ||
6 | EVGFP37+HRI | 1 | 90.6 ± 5.2 (85.4; 95.8) | 21.6 (17.1; 26.2) |
4 | 19.4 (17.6; 21.2)# | 21.9 (18.0; 25.8) | ||
7 | 0.5 (0.2; 0.8) | 10.5 (8.4; 12.6) | ||
14 | 0.2 (0.1; 0.3) | 2.3 (1.9; 2.7) | ||
7 | Control (EV) | 0 | 0 | |
Note. * — significant differences (p < 0.05) with group 1 on the corresponding day; # –– significant differences (p < 0.05) between groups 1 and 4, 2 and 5, 3 and 6 on the corresponding day.
In the EVGFP37+HRI group, the PI was registered at the level of the analogous index in the EVGFP37 group. At the same terms (4th day) in the EVGFP37+AB group the PI was significantly increased (p < 0.05) in comparison with the analogous index in the EVGFP37 group. A significant increase of the PN in EVGFP28+AB group on the 4th and 7th days, and in EVGFP28+HRI group — on the 7th day in comparison with this index in EVGFP28 group was revealed (p < 0.05).
Next, we determined the effect of EVGFP cultivation temperature on the ability of guinea pig spleen phagocytes to engulf and digest cells of the fluorescent strain. In the EVGFP37+AB and EVGFP37+HRI groups at day 4, the PI values were 2-fold higher (p < 0.05) than in the EVGFP28+AB and EVGFP28+HRI groups, respectively. In the EVGFP37 group on the 4th day the PN was 1.5 times higher (p < 0.05) than in the EVGFP28 group on average.
Discussion
The preclinical stage of evaluation of live plague vaccines should not only demonstrate that the vaccine is immunogenic and has protective efficacy, but also substantiate the safety of the preparation, primarily related to the degree of residual virulence (harmlessness) of the vaccine strain of the plague microbe, characterized by its ability to spread and prolonged persistence in the organs of biomodels.
Cell engraftment of the biofluorescent strain was studied in guinea pig organs by microscopic and flow cytometric methods for 14 days, which corresponds to the acceptable period of cell reproduction of the Y. pestis vaccine strain EV NIIEG, which causes immunological reorganization of the organism (non-sterile phase of immunity) [12].
The method of fluorescence microscopy, one of the main optical methods of fluorescence visualization [22], makes it possible to clearly and efficiently assess the stage of virulent strain spreading in organs and tissues of white mice [4]. In our studies, the established visualization of EVGFP in smear-prints from the site of culture administration in all experimental groups on the 1st day of the immune response is consistent with the results of earlier quantitative bacteriological studies, in which the highest number of cells of the Y. pestis vaccine strain EV NIIEG were found at the injection site (2.3 × 107 m.c./g) after 24 h [12].
The absence of fluorescent microbial cells on the 4th, 7th, and 14th days of immunogenesis is probably due to the low concentration of EVGFP in the smear-prints (˂ 105 m.c./ml), lying beyond the lower threshold of 105 m.c./mL sensitivity of fluorescent microscopy [23].
New opportunities were opened by the use of a more sensitive and productive technology of flow cytofluorimetric analysis, which allows to control in vivo survival of bacteria in phagocytes, as well as to monitor their distribution in the host organism in dynamics [11, 24]. Phagocytes containing fluorescent bacterial cells were recorded for 4 days. The decrease in the number of fluorescent phagocytes (by the 4th day on average 4.4 times as compared to the 1st day) could be associated with both intracellular digestion of ingested bacteria and a decrease in the absorption capacity of phagocytes towards plague microbes in the active growth stage in vivo at the temperature of the host organism. Intracellular localization of EVGFP in macrophages and neutrophils of spleen was confirmed by similar results obtained by foreign scientists by flow cytometry in experiments with another fluorescent strain of Y. pestis (pAGFP) expressing GFP [11]. The sample preparation procedure we used (Lyse/No-wash) without washing splenocytes from the erythrocyte lysing and leukocyte fixing FACS Lysing Solution actually completely excluded bacterial adhesion on the cell surface, since the solutions used for erythrocyte lysis remove bacteria adsorbed on the surface of formaldehyde-fixed leukocytes [19].
The use of biofluorescent strain and flow cytofluorimetric technology allowed us to register the different effect of immunomodulatory drugs used in this work on the outcome of interaction of the studied EVGFP strain with phagocytes of guinea pig spleen.
The obtained data on the combined use of AB with the vaccine strain, based on the analysis of phagocytic activity of macrophages and neutrophils of guinea pig spleen in our experiment, confirmed the previously revealed fact of the stimulating effect of AB on the phagocytic activity of blood leukocytes of BALB/c mice in relation to Y. pestis EV NIIEG in in vitro tests [15].
According to the literature data on immunological similarity in IFN-γ genetic expression patterns and amino acid sequence homology between guinea pig and human [25, 26], HRI had a different effect on the phagocytosis process, decreasing the PI and increasing the PN (number of microbial cells per phagocyte) at 28°C. This increase could be explained by the assumption of the ability of HRI to inhibit intracellular digestion of bacteria in phagocytes. However, this explanation is contradicted by the known ability of recombinant IFN-γ to activate macrophages and cause the death of intracellular microorganisms [27]. Consequently, this fact is explained by the effect of IFN-γ on the properties of the vaccine strain, leading to a decrease in its engraftment in the macroorganism.
In experiments with the use of biofluorescent strain cultures grown in different temperature regimes for vaccination, the known fact of longer survival and digestion of 37°C Y. pestis culture cells in macrophages was confirmed [28, 29], associated with the induction of expression of Caf1 (F1) and other antiphagocytic factors that block phagocytosis: outer membrane protein Ail, plasminogen activator Pla, PsaA (pH6 antigen) [11, 30, 31].
Conclusion
On the example of application of biofluorescent Y. pestis vaccine strain EV NIIEG pTurboGFP-B and the method of flow cytometry showed the possibility of increasing the efficiency of assessment of strain engraftment in the macroorganism, and the use of cytofluorimetric technology increases its informativity and objectivity, including due to the speed of such analysis, allowing to perform additional studies that reveal the mechanisms of interaction between the micro- and macroorganism.
About the authors
Svetlana N. Klyueva
Russian Anti-Plague Institute "Microbe"
Author for correspondence.
Email: klyueva.cvetlana@mail.ru
ORCID iD: 0000-0002-5550-6063
Cand. Sci. (Biol.), researcher, Department of immunology
Russian Federation, SaratovAngelina A. Budanova
Russian Anti-Plague Institute "Microbe"
Email: klyueva.cvetlana@mail.ru
ORCID iD: 0000-0002-5092-432X
Cand. Sci. (Biol.), senior researcher, Department of immunology
Russian Federation, SaratovAleksandr L. Kravtsov
Russian Anti-Plague Institute "Microbe"
Email: kravzov195723@gmail.com
ORCID iD: 0000-0002-9016-6578
Sci. (Biol.), leading researcher, Department of immunology, Russian Anti-Plague Institute "Microbe"
Russian Federation, SaratovSvetlana A. Bugorkova
Russian Anti-Plague Institute "Microbe"
Email: klyueva.cvetlana@mail.ru
ORCID iD: 0000-0001-7548-4845
Sci. (Med.), chief researcher, Department of immunology, Russian Anti-Plague Institute "Microbe"
Russian Federation, SaratovReferences
- Chacón-Díaz C., Zabalza-Baranguá A., San Román B., et al. Brucella abortus S19 GFP-tagged vaccine allows the serological identification of vaccinated cattle. PLoS One. 2021;16(11):e0260288. DOI: https://doi.org/10.1371/journal.pone.0260288
- Gensberger E.T., Kostić T. Green fluorescent protein labeling of food pathogens Yersinia enterocolitica and Yersinia pseudotuberculosis. J. Microbiol. Methods. 2017;132:21–6. DOI: https://doi.org/10.1016/j.mimet.2016.11.008
- Куклева Л.М., Тучков И.В., Оглодин Е.Г. и др. Получение штамма Yersinia pestis, продуцирующего флуоресцентный белок GFP, и перспективы его использования. Проблемы особо опасных инфекций. 2019;(4):61–6. Kukleva L.M., Tuchkov I.V., Oglodin E.G., et al. Construction of Yersinia pestis strain producing fluorescent protein GFP and prospects of its usage. Problems of Particularly Dangerous Infections. 2019;(4):61–6. DOI: https://doi.org/10.21055/0370-1069-2019-4-61-66 EDN: https://elibrary.ru/kprnki
- Макашова М.А., Морозов О.А., Оглодин Е.Г. и др. Набор рекомбинантных флуоресцентных штаммов бактерий вида Yersinia pestis античного биовара основного подвида и алтайского биовара центральноазиатского подвида для индикации возбудителя чумы в экспериментальных образцах. Патент РФ № 2769790С1;2022. Makashova M.A., Morozov O.A., Oglodin E.G., et al. Set of recombinant fluorescent strains of Yersinia pestis bacteria of main subspecies biovar and the Altai biovar of the central Asiatic subspecies for indication of plague agent in experimental samples. Patent RF № 2769790С1; 2022.
- Lemon A., Sagawa J., Gravelle K., Vadyvaloo V. Biovar-related differences apparent in the flea foregut colonization phenotype of distinct Yersinia pestis strains do not impact transmission efficiency. Parasit. Vectors. 2020;13(1):335. DOI: https://doi.org/10.1186/s13071-020-04207-x
- Bi Y., Du Z., Han Y., et al. Yersinia pestis and host macrophages: immunodeficiency of mouse macrophages induced by YscW. Immunology. 2009;128(1 Pt. 2):e406–17. DOI: https://doi.org/10.1111/j.1365-2567.2008.02990.x
- Bi Y., Wang X., Han Y., et al. Yersinia pestis versus Yersinia pseudotuberculosis: effects on host macrophages. Scand. J. Immunol. 2012;76(6):541–51. DOI: https://doi.org/10.1111/j.1365-3083.2012.02767.x
- Born F., Braun P., Scholz H.C., Grass G. Specific detection of Yersinia pestis based on receptor binding proteins of phages pathogens. Pathogens. 2020;9(8):611. DOI: https://doi.org/10.3390/pathogens9080611
- Su S., Bangar H., Saldanha R., et al. Construction and characterization of stable, constitutively expressed, chromosomal green and red fluorescent transcriptional fusions in the select agents, Bacillus anthracis, Yersinia pestis, Burkholderia mallei and Burkholderia pseudomallei. Microbiologyopen. 2014;3(5):610–29. DOI: https://doi.org/10.1002/mbo3.192
- Shchelkunov S.N., Yakubitskiy S.N., Titova K.A., et al. Enhancing the protective immune response to administration of a LIVP-GFP live attenuated Vaccinia virus to mice. Pathogens. 2021;10(3):377. DOI: https://doi.org/10.3390/pathogens10030377
- Lukaszewski R.A., Kenny D.J., Taylor R., et al. Pathogenesis of Yersinia pestis infection in BALB/c mice: effects on host macrophages and neutrophils. Infect. Immun. 2005;73(11):7142–50. DOI: https://doi.org/10.1128/iai.73.11.7142-7150.2005
- Самойлова Л.В., Пионтковский С.А., Плотникова Е.А. и др. Особенности размножаемости вирулентного и вакцинного штаммов чумного микроба в организме морских свинок. В кн.: Горькова А.В., ред. Профилактика особо опасных инфекций. Саратов;1988:3–13. Samoilova L.V., Piontkovskii S.A., Plotnikova E.A., et al. Peculiarities of multiplication of virulent and vaccine strains of the plague microbe in the body of guinea pigs. In: Gor'kova A.V., ed. Prevention of Especially Dangerous Infections. Saratov;1988:3–13.
- Андрюков Б.Г., Сомова Л.М., Тимченко Н.Ф., Исследование температурозависимых молекулярных механизмов развития инфекций — ключ к созданию современных профилактических средств (обзор). Современные технологии в медицине. 2016;8(3):137–50. Andryukov B.G., Somova L.A., Timchenko N.F. The study of temperature-dependent molecular mechanisms of infection development as a key to the development of modern prophylactic drugs (review). Modern Technologies in Medicine. 2016;8(3):137–50. DOI: https://doi.org/10.17691/stm2016.8.3.16 EDN: https://elibrary.ru/xqnhmn
- Кравцов А.Л., Курылина А.Ф., Клюева С.Н., Щуковская Т.Н. Модулирующий эффект полиоксидония на реактивность клеток иммунной системы при формировании противочумного иммунитета. Иммунология. 2016;37(6):320–5. Kravtsov A.L., Curylina A.F., Klyueva S.N., Shchukovskaya T.N. The modulating effect of polyoxidonium on the reactivity of immune cells in the formation of anti-plague immunity. Immunology. 2016;37(6):320–5. DOI: https://doi.org/10.18821/0206-4952-2016-37-6-320-325 EDN: https://elibrary.ru/xipgkh
- Клюева С.Н., Кравцов А.Л., Бугоркова С.А. и др. Фагоцитарная и цитокин-продуцирующая активность лейкоцитов крови мышей линии BALB/c, привитых против чумы на фоне иммуномодуляции полиоксидонием. Российский иммунологический журнал. 2019;13(4):1412–20. Klyueva S.N., Kravtsov A.L., Bugorkova S.N., et al. Blood leukocyte phagocytic and cytokine-producing activity of anti-plague vaccinated BALB/c line mice against the background of immunomodulation by polyoxidonium. Russian Journal of Immunology. 2019;13(4):1412–20. EDN: https://elibrary.ru/aqjuec
- Гончарова А.Ю., Бугоркова С.А., Кудрявцева О.М. и др. Экспериментальная оценка эффективности применения вакцинного штамма Yersinia pestis EV НИИЭГ в сочетании с иммуномодуляторами. Проблемы особо опасных инфекций. 2020;(2):71–7. Goncharova A.Yu., Bugorkova S.A., Kudryavtseva O.M., et al. Experimental evaluation of application of the vaccine strain Yersinia pestis EV NIIEG in combination with immune-modulators. Problems of Particularly Dangerous Infections. 2020;(2):71–7. DOI: https://doi.org/10.21055/0370-1069-2020-2-71-77, EDN: https://elibrary.ru/fbjedk
- Conchas R.F., Carniel E. A highly efficient electroporation system for transformation of Yersinia. Gene. 1990;87(1):133–7. DOI: https://doi.org/10.1016/0378-1119(90)90505-l
- Spinner J.L., Winfree S., Starr T., et al. Yersinia pestis survival and replication within human neutrophil phagosomes and uptake of infected neutrophils by macrophages. J. Leukoc. Biol. 2014;95(3):389–98. DOI: https://doi.org/10.1189/jlb.1112551
- Кравцов А.Л., Клюева С.Н., Кожевников В.А. и др. Влияние противочумной вакцинации на фагоцитарную активность гранулоцитов крови человека. Российский иммунологический журнал. 2021;24(1):113–22. Kravtsov A.L., Klyueva S.N., Kozhevnikov V.A., et al. Effect of antiplague vaccination on phagocytic activity of human blood granulocytes. Russian Journal of Immunology. 2021;24(1):113–22. DOI: https://doi.org/10.46235/1028-7221-166-EOA, EDN: https://elibrary.ru/aibbvs
- Олиферук Н.С., Пинегин Б.В. Определение фагоцитарного числа лейкоцитов периферической крови по отношению к Staphylococcus aureus с помощью проточной цитометрии. Иммунология. 2007;28(4):236–40. Oliferuk N.S., Pinegin В.V. The phagocytic number definition of peripheral blood leukocytes in the ratio Staphylococcus aureus with flowing cytofluorimetry. Immunology. 2007;28(4):236–40. EDN: https://elibrary.ru/iatzdj
- White-Owen C., Alexander J.W., Sramkoski R.M., Babcock G.F. Rapid whole-blood microassay using flow cytometry for measuring neutrophil phagocytosis. J. Clin. Microbiol. 1992;30(8):2071–6. DOI: https://doi.org/10.1128/jcm.30.8.2071-2076.1992
- Ведяйкин А.Д., Ходорковский М.А., Вишняков И.Е. Методы флуоресцентной микроскопии сверхвысокого разрешения и их использование для визуализации различных клеточных структур. Цитология. 2019;61(5):343–56. Vedyaykin A.D., Khodorkovskii M.A., Vishnyakov I.E. Super-resolution microscopy methods and their use for visualization of various cell structures. Cytology. 2019;61(5):343–56. DOI: https://doi.org/10.1134/S0041377119050067, EDN: https://elibrary.ru/unjbeu
- Онищенко Г.Г., Кутырев В.В., ред. Лабораторная диагностика опасных инфекционных болезней. Практическое руководство. М.;2013. Onishchenko G.G., Kutyrev V.V., eds. Laboratory Diagnostics of Dangerous Infectious Diseases. Practical Guide. Moscow;2013.
- Tartaro K., VanVolkenburg M., Wilkie D., et al. Development of a fluorescence-based in vivo phagocytosis assay to measure mononuclear phagocyte system function in the rat. J. Immunotoxicol. 2015;12(3):239–46. DOI: https://doi.org/10.3109/1547691x.2014.934976
- Yamada H., Udagawa T., Mizuno S., et al. Newly designed primer sets available for evaluating various cytokines and iNOS mRNA expression in guinea pig lung tissues by RT-PCR. Exp. Anim. 2005;54(2):163–72. DOI: https://doi.org/10.1538/expanim.54.163
- Jeevan A., Yoshimura T., Lee K.E., McMurray D.N. Differential expression of gamma interferon mRNA induced by attenuated and virulent Mycobacterium tuberculosis in guinea pig cells after Mycobacterium bovis BCG vaccination. Infect. Immun. 2003;71(1):354–64. DOI: https://doi.org/10.1128/iai.71.1.354-364.2003
- Сологуб Т.В., Цветков В.В., Деева Э.Г. Интерферон гамма-цитокин с противовирусной, иммуномодулирующей и противоопухолевой активностью. Российский медико-биологический вестник имени академика И.П. Павлова. 2014;22(3):56–60. Sologub T.V., Tsvetkov V.V., Deeva E.G. Interferon gamma-cytokine with antiviral, immunomodulatory and antitumor action. I. P. Pavlov Russian Medical Biological Herald. 2014;22(3):56–60. DOI: https://doi.org/10.17816/pavlovj2014356-60 EDN: https://elibrary.ru/szvbxl
- Du Y., Rosqvist R., Forsberg A. Role of fraction 1 antigen of Yersinia pestis in inhibition of phagocytosis. Infect. Immun. 2002;70(3):1453–60. DOI: https://doi.org/10.1128/iai.70.3.1453-1460.2002
- Ke Y., Chen Z., Yang R. Yersinia pestis: mechanisms of entry into and resistance to the host cell. Front. Cell. Infect. Microbiol. 2013;3:106. DOI: https://doi.org/10.3389/fcimb.2013.00106
- Подладчикова О.Н. Современные представления о молекулярных механизмах патогенеза чумы. Проблемы особо опасных инфекций. 2017;(3):33–40. Podladchikova O.N. Modern views on molecular mechanisms of plague pathogenesis. Problems of Particularly Dangerous Infections. 2017;(3):33–40. DOI: https://doi.org/10.21055/0370-1069-2017-3-33-40, EDN: https://elibrary.ru/zhgvxr
- Peters D.T., Reifs A., Alonso-Caballero A., et al. Unraveling the molecular determinants of the anti-phagocytic protein cloak of plague bacteria. PLoS Pathog. 2022;18(3):e1010447. DOI: https://doi.org/10.1371/journal.ppat.1010447
Supplementary files