Adaptation of H2N2 influenza viruses with different receptor specificity to MDCK cells: opportunities for the development of a cell-based vaccine against pandemic H2N2 influenza
- Authors: Matyushenko V.A.1, Kostromitina A.D.1, Rudenko L.G.1, Isakova-Sivak I.N.1
-
Affiliations:
- Institute of Experimental Medicine
- Issue: Vol 102, No 1 (2025)
- Pages: 31-42
- Section: ORIGINAL RESEARCHES
- URL: https://microbiol.crie.ru/jour/article/view/18803
- DOI: https://doi.org/10.36233/0372-9311-624
- EDN: https://elibrary.ru/zffqga
- ID: 18803
Cite item
Abstract
Introduction. H2N2 influenza viruses caused a pandemic in 1957 due to the adaptation of avian influenza hemagglutinin from avian-type α2,3 to human-type α2,6 receptor specificity. These viruses have not circulated among humans for more than 50 years but are still found in avian reservoirs, indicating their pandemic potential. It is known that at the beginning of a pandemic wave, viruses with α2,3 and α2,6 receptor specificities can co-circulate, and the selection of one or another isolate for the development of a better pandemic influenza vaccine should be based on strong scientific evidence. Although the vast majority of influenza vaccines are produced in chicken embryos, mammalian cell culture may be a preferred substrate for the production of pandemic influenza vaccines.
Materials and methods. In this study, we investigated two variants of A/Singapore/1/57 (H2N2) virus which differed by their receptor specificity defined by three residues in the HA1 molecule: E156, Q226, G228 for α2,3 avian-type (Sing-α2,3) and K156, L226, S228 for α2,6 human-type (Sing-α2,6) receptor specificity. We conducted serial passaging of these viruses on MDCK cells and analyzed growth properties of plaque-purified clones in vitro and in vivo, as well as their immunogenicity and cross-reactivity in a mouse model.
Results. Adaptation to MDCK cells significantly increased viral titers in MDCK cells; however, their receptor specificity was not affected. Viruses with α2,6 receptor specificity induced higher titers of homologous antibodies compared to the viruses with α2,3 receptor specificity, but these antibodies could react only with the α2,6 viruses. In contrast, antibody induced by viruses with α2,3 receptor specificity had broad reactivity against all studied viruses. Similar results were obtained for the pair of A/Leningrad/17-based H2N2 live attenuated influenza vaccines with α2,3 and α2,6 receptor specificities in experiments on Syrian hamsters.
Conclusion. In the case of a new transmission of H2N2 avian influenza viruses to the human population and co-circulation of viruses with both receptor specificities, the variant with α2,3 specificity should be selected for the development of cross-reactive influenza vaccines.
Full Text
Introduction
Avian influenza is a zoonotic infection that poses a high risk to humans due to the high mortality rate, which reaches 60% when infected with highly pathogenic subtypes H5N1, H7N9, H5N6 and H10N8 [1–4]. Asian influenza subtype H2N2 appeared in Singapore in February 1957 and rapidly caused a pandemic that claimed more than 2.7 million lives. The H2N2 influenza pandemics in 1957 and H3N2 in 1968 are known to have been caused by a switch in the receptor specificity of the virus from avian sialic receptor α2,3 to human α2,6, with influenza viruses with both types of receptor specificity circulating simultaneously at the beginning of the pandemic wave [5, 6]. Since birds are the main reservoir and carry almost all known subtypes of influenza A virus, including H2N2, the risks of these viruses returning to circulation among humans are estimated to be quite high [7]. Given the decline in population immunity to H2N2 viruses due to their prolonged absence from circulation, scientists around the world are calling for vaccination campaigns against these viruses to be launched in advance, without waiting for the onset of the pandemic [8].
Influenza vaccine prophylaxis is known to be the optimal method of controlling this infection, and there are many influenza vaccines available for seasonal administration. However, in pandemic settings, live attenuated influenza vaccine (LAIV) is considered the most effective [9, 10]. The vast majority of influenza vaccines in the world are produced in embryonated chicken eggs, but in recent decades there has been an active discussion of transferring the production of influenza vaccines to mammalian cell cultures, which would allow for the short-term production of large amounts of viral biomass, as well as narrowing the list of contraindications, in particular, allowing the vaccine to be administered to persons allergic to chicken protein [11]. Furthermore, if an influenza pandemic is caused by a highly pathogenic virus, there is a high probability that the chicken population in poultry farms will be completely destroyed, so the independence of vaccine production from the supply of eggs from poultry farms is also extremely important. Thus, it is advisable to transfer influenza vaccine production to MDCK cell culture, since numerous studies show that it is in this cell culture that vaccine strains of LAIV are able to replicate to titers comparable to those of eggs [12–14].
The main aim of this study was to find the most promising variant of the vaccine strain of LAIV A(H2N2) culture that should be used at the beginning of the pandemic wave. For this purpose, two variants of the pandemic virus strain A/Singapore/1/57 (H2N2) differing in receptor specificity and LAIV strains prepared on their basis were studied. Adaptation of the viruses to MDCK cell line was performed, followed by cloning by the plaque assay and evaluation of the receptor specificity of the isolated virus variants. The variants differing in the HA gene sequences were used for immunization of laboratory animals to reveal the potential effect of adaptive mutations in virus surface proteins on immunogenicity, antigenicity and cross-reactivity of antibodies produced after immunization.
Materials and methods
Viruses
Two variants of pandemic virus strain A/Singapore/1/57 (H2N2) obtained from the collection of the Department of Virology of Institute of Experimental Medicine were used, which differed in sensitivity to nonspecific serum inhibitors. Experiments with live H2N2 viruses were conducted in the laboratory with a biosafety level of BSL-3.
Production of LAIV strains by reverse genetics methods
Hemagglutinin and neuraminidase genes were cloned into the pCIPolISapIT vector for reverse genetics using universal primers specific for each gene in reverse transcription polymerase chain reaction [15]. A set of 6 plasmids with bidirectional reads encoding internal proteins of the attenuation donor A/Leningrad/134/17/57 (H2N2) was prepared previously [16]. Live influenza viruses were obtained by electroporation of Vero cells using the Neon transfection system (Invitrogen) and the accompanying 100 μl Neon Kit.
Hemagglutination reaction
The hemagglutination assay (HA) was performed according to the classical scheme using chicken red blood cells (RBC)1. To investigate the receptor specificity of influenza viruses, we used a modified HA with the exo-α-Sialidase enzyme (Salmonella typhimurium) (Megazyme), which cleaves exclusively α2,3-receptors from the RBC surface. Horse RBC, which express only α2,3-receptors on their surface; untreated chicken RBC, which express both types of receptors; and chicken RBC treated with exosialidase for 1 h at 37ºC, i.e., carrying only α2,6-receptors on their surface, were used for HA.
The virus was considered to have α2,3-receptor specificity if its titer in HA with horse and chicken RBC was the same and its titer in HA with treated chicken RBC was 0. Otherwise, the virus was considered to have α2,6-receptor specificity. If the titer was positive in all HA, the virus was considered to have dual receptor specificity with preference for the type with the higher titer in HA.
Growth of viruses and determination of infectious titer
To accumulate influenza viruses in 10–11-day-old embryonated chicken eggs, that were infected with 0.2 ml of viral material, after which the eggs were incubated for 48–72 h at 33–37ºC. Virus propagation in MDCK cells was performed on a daily monolayer with 90–95% confluency grown in DMEM medium supplemented with 1× antimycotic antibiotic (Gibco) and 10% fetal bovine serum (Biolot) at 37ºC in a thermostat containing 5% CO2. To infect MDCK cells, the prepared monolayer was washed twice with a warm solution of phosphate buffered saline(PBS), after which the viral suspension was added in volumes of 1, 2, 3 ml into vials T-25, T-75 and T-175, respectively. After incubation for 1 h at 33ºC for vaccine strains and 37ºC for wild-type influenza viruses in a thermostat containing 5% CO2, the inoculum was removed and DMEM medium with 1×antibiotic-antimycotic and 1 μg/mL TPCK trypsin (Sigma-Aldrich Co.) was added. After 72 h of incubation at 33ºC or 37ºC, the cytopathic effect (CPE) of the virus was visually assessed and its titer was determined by HA.
Infection titers of viruses in both culture systems were determined by the limit dilution method. Eggs were infected with 10-fold serial dilutions of viruses in 200 μL PBS and incubated at 33ºC and 37ºC for 48 h, after which the presence of virus was determined by HA with chicken erythrocytes. Titer determination in MDCK cells was performed on 96-well plates with a daily monolayer, and serial 10-fold dilutions were prepared on DMEM medium with antibiotic-antimycotic and 1 μg/mL of TPCK trypsin. After adsorption, the inoculum was removed, cells were washed and incubated in maintenance medium for 3 days. The presence of viruses in the wells was determined by HA with chicken RBC. Virus titers in eggs and MDCK cells were calculated according to the method of Reed and Mench [17] and expressed in 50% embryonic (log10 EID50/mL) and tissue cytopathogenic (log10 TCID50/mL) infectious doses.
Adaptation of viruses to MDCK cells
Adaptation of influenza viruses to MDCK cells was performed by sequential 5-fold passaging of strains followed by virus cloning by the plaque assay and isolation of viral clones from individual plaques. For this purpose, 10-fold dilutions of viruses in 2 repeats were applied to 6-well plates seeded the day before with MDCK cells. After one hour of contact with regular shaking, the inoculum was removed, and 3 ml of agarose coating obtained by mixing equal volumes of 2×DMEM medium (in the presence of AbAm and 2 μg/ml TPCK trypsin) and 1.6% fusible agarose (Lonza) were added to the wells. On day 3-5 of incubation, viral plaques were visually assessed, 20–30 well-separated plaques were isolated on limiting dilutions, a separate virus clone was isolated from each individual plaque, which was grown on MDCK cells. Complete nucleotide sequences of surface protein genes were obtained by the Sanger method using the BigDye Terminator Cycle Sequencing Kit v. 3.1 (Thermo).
Experiments with laboratory animals
In animal experiments, mice of the CBA line and Syrian hamsters (Stolbovaya, Russia) were used. The study was approved by the Ethical Committee of the Institute of Experimental Medicine (protocol No. 1/20 of 27.02.2020).
To evaluate the immunogenicity of wild influenza viruses with different receptor specificity, female mice of the CBA line were infected intranasally at a dose of 105 EID50/animal. After 21 days, the animals were euthanized, after which blood sera and upper respiratory tract (URT) washes were collected to determine the level of humoral immune response to different virus variants. To evaluate the immunogenicity of the vaccine strains of H2N2 LAIV, Syrian hamsters were immunized intranasally at a dose of 105 EID50/animal, twice 21 days apart. On the 21st day after the 2nd immunization, animals were euthanized, blood serum, URT washes and bronchoalveolar lavage were collected.
Immunological methods
The study of animal blood sera in hemagglutination inhibition assay (HAI) was performed according to the standard protocol2 with chicken RBC and treatment of sera with receptor-destroying enzyme (RDE, Denka). The last dilution at which complete inhibition of hemagglutination assay counted as the serum titer in HAI.
Enzyme immunoassay
An enzyme-linked immunosorbent assay (ELISA) with animal samples was performed using influenza viruses, purified in sucrose density gradient, as antigen. Antigen was added to 96-well high sorption plates (Corning) at 16 AU in 50 μL and incubated overnight at 4ºC. The plates were washed 3 times with wash buffer (phosphate-salt buffer + 0.05% Twin-20 (Biolot)), after which unbound sites were blocked with 1% bovine serum albumin.
Double dilutions of sera or respiratory tract washes were prepared in separate round-bottom plates, which were then transferred to the wells of the plate washed from the blocking solution. After incubation for 1 h at 37°C, the plates were again washed 3 times with wash buffer, dried and horseradish peroxidase-conjugated secondary antibodies: mouse anti-IgG (1:10 000), mouse anti-IgA (1:2000), hamster anti-IgG (1:5000) and hamster anti-IgA (1:300) were added. The plate was incubated for 1 h at 37ºC, after which the plate was washed 5 times with wash buffer, dried and 50 μl/well of TMB substrate (Thermo) was added and incubated in the dark for up to 20 min at room temperature. The reaction was stopped by adding 50 μl of 1M H2SO4. The primary ELISA results were measured on a spectrophotometer (Bio-Rad) at a wavelength of 450 nm. The last dilution at which the optical density exceeded twice the average of the control wells was taken as the antibody titer. The area under the optical density curve was calculated using the GraphPad Prism 7 software package.
Statistical processing of data
For data comparison, non-parametric Mann-Whitney U-test; Student's t-test and ANOVA using GraphPad Prism 7 software were used. Differences were considered reliable at p < 0.05.
Results
Two variants of the pandemic strain A/Singapore/1/57 (H2N2) were recovered from ampoules of viral material lyophilized in 1975, and the exact passaging history of the viruses is unknown. The viruses was grown in eggs differed in their level of sensitivity to nonspecific guinea pig serum inhibitors. Whole-genome sequencing showed that these viruses had amino acid differences at positions 156 (E/K), 226 (Q/L), and 228 (G/S) in the HA1 subunit (Table). According to the literature, substitutions at positions 226 and 228 are responsible for the receptor specificity of influenza virus [5, 6]. It is without a doubt that the evaluation of the affinity of these viruses for receptors on the erythrocyte surface in HA with different types of RBC showed that the virus with amino acid residues E156, Q226 and G228 has α2,3-receptor specificity (designated Sing-α2,3), while the variant with residues K156, L226 and S228 has affinity for α2,6-receptors (Sing-α2,6) (Fig. 1, a). The amino acid substitution K19T was found in the neuraminidase molecule, but since it is located in the transmembrane domain, it has no effect on receptor specificity (Table). Adaptation of the studied viruses to MDCK cells and subsequent cloning by plaque allowed the isolation of 3 additional virus variants with different HA sequences: Sing-α2,6-EP with G158E and L321P mutations in the HA1 subunit, Sing-α2,3-S with P221S mutation in the HA1 subunit, and Sing-α2,3-V with A96V mutation in the HA2 subunit (Table).
Amino acid substitutions in surface proteins of investigated variants of A/Singapore/1/57 (H2N2) virus
Virus | HA | NA | ||||||
HA1 | HA2 | |||||||
156 | 158 | 221 | 226 | 228 | 321 | 96 | 19 | |
Original strains accumulated in the Egg | ||||||||
Sing-α2,6 | Lys | Gly | Pro | Leu | Ser | Leu | Ala | Thr |
Sing-α2,3 | Glu | Gly | Pro | Gln | Gly | Leu | Ala | Lys |
MDCK-adapted strains | ||||||||
Sing-α2,6-EP | Lys | Glu | Pro | Leu | Ser | Pro | Ala | Thr |
Sing-α2,3-S | Glu | Gly | Ser | Gln | Gly | Leu | Ala | Lys |
Sing-α2,3-V | Glu | Gly | Pro | Gln | Gly | Leu | Val | Lys |
Fig. 1. Characterization of the studied viruses in vitro.
a — titers of viruses in HA with untreated chicken erythrocytes (1), horse erythrocytes (2) and chicken erythrocytes treated with exosialidase (3); b — infectious activity of the studied viruses in the Egg and MDCK cells.
Examination of MDCK-adapted variants in HA showed that the Sing-α2.6-EP strain has affinity for α2,6 receptors, while the Sing-α2,3-S and Sing-α2,3-V variants have affinity for α2,3 receptors (Fig. 1, a). Thus, adaptation of wild-type H2N2 influenza viruses to mammalian cell culture does not significantly affect their receptor specificity.
In addition, the infectious activity of all viruses in eggs and MDCK cells was studied. It was found that Sing-α2,3 virus was on average 2 orders higher in eggs than Sing-α2,6 virus, while their titers in MDCK cells were comparable (Fig. 1, b). Importantly, the infectious activity of MDCK-adapted variants in cell culture was significantly higher than that of the corresponding original viruses. Thus, the contribution of mutations G158E and L321P, P221S in the HA1 and A96V in the HA2 subunits to the increase in the infectious titer of the virus in MDCK cells was observed (Fig. 1, b).
Immunization of CBA mice with the original Sing-α2.6 and Sing-α2,3 strains and MDCK-adapted variants induced higher levels of homologous serum antibodies to Sing-α2.6 and Sing-α2.6-EP viruses compared with viruses with affinity for α2.3 receptors (Fig. 2, a, b). At the same time, cell-adapted Sing-α2,3-S and Sing-α2,3-V variants induced significantly lower levels of homologous serum IgG antibodies compared with the original Sing-α2,3 variant (Fig. 2, b). Examination of the local humoral immune response showed significant increases in secretory IgA antibodies in all 5 viruses tested: Sing-α2,6, Sing-α2,6-EP, Sing-α2,3, Sing-α2,3-S and Sing-α2,3-V (Fig. 2, c). Comparison of IgA antibody levels in the original Sing-α2,6 and Sing-α2,3 virus groups showed no differences (p = 0.3355), which is in contrast to the data on the systemic humoral response. Nevertheless, a comparative analysis of the levels of secretory IgA antibodies between groups of animals infected with MDCK-adapted variants of Sing-α2,6-EP, Sing-α2,3-S, and Sing-α2,3-V, as well as in the systemic response, revealed the superiority of Sing-α2,6-EP virus. Summarizing the data on the induction of systemic and local immune response by the studied viruses, we can conclude that all the viruses induce humoral response, but the MDCK-adapted variants with α2,3 receptor specificity (Sing-α2,3-S and Sing-α2,3-V) were the least immunogenic at the level of both systemic and local humoral immunity. On the contrary, Sing-α2,6, Sing-α2,6-EP viruses with α2,6 receptor specificity did not differ in immunogenicity in any of the tests.
Fig. 2. Assessment of humoral immune response to a single administration of the tested viruses to CBA mice.
a — level of homologous serum antibodies detected in HAI; b — level of homologous serum IgA antibodies in ELISA; c — level of homologous secretory IgG antibodies in ELISA.
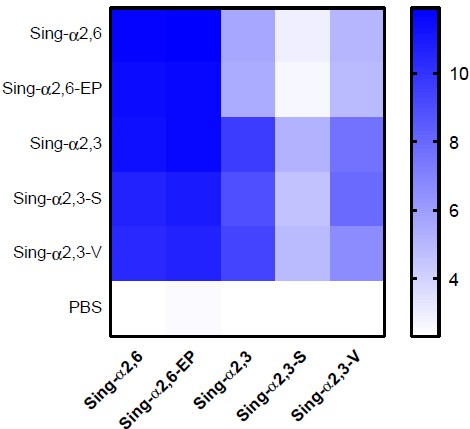
Further, the cross-reactivity of serum antibodies produced by administration of 5 tested variants of A/Singapore/1/57 (H2N2) virus was evaluated against each variant in HAI and ELISA. Interestingly, when viruses with α2-6-receptor specificity were used as antigens in HAI, significantly higher antibody titers were detected in all immunized groups compared with antigens with α2-3 specificity (Fig. 3, a). However, antibodies in the sera of the Sing-α2.6 group did not bind any of virus variants with α2-3-receptor specificity. Although antibody titers above the detection level were detected in mice immunized with the MDCK-adapted Sing-α2,6-EP variant, no statistically significant differences compared to the control group were found. The study of cross-reactivity of serum IgG antibodies by ELISA showed similar results: viruses with α2-6-receptor specificity as antigens revealed the highest values of antibody titers in all groups, whereas antibody binding to viruses with α2,3-receptor specificity was significantly weaker in animals of all groups (Fig. 3, b).
Fig. 3. Heat map of the immunogenicity and cross-reactivity of investigated variants of A/Singapore/1/57 (H2N2) virus in the experiment on mice (n = 7).
a — mean values of the levels of anti-hemagglutinating antibodies in all immunized groups against different viral antigens; b — mean values of the levels of serum IgG antibodies in all immunized groups against different viral antigens.
It is important to note that viruses with α2-6-receptor specificity as antigen bound antibodies equally well in the sera of mice from all groups studied, except for the group of animals immunized with Sing-α2,3-V virus, in which antibody titers to Sing-α2,6 and Sing-α2,6-EP viruses differed significantly from those in the other groups (Fig. 3, a). The opposite situation was observed in groups of animals immunized with MDCK-adapted variants with α2-3-receptor specificity: IgG antibody titers to Sing-α2,3-S and Sing-α2,3-V viruses were reduced in all immunized groups; while the P221S substitution in the HA1 subunit could be characterized as an escape mutation, since Sing-α2,3-S virus escapes antibody recognition most efficiently in all immunogenic variants studied (Fig. 3, b).
Overall, the results indicate that variants with α2-3-receptor specificity adapted to or isolated on MDCK cell culture are the most suitable viruses for the production of a cell-based H2N2 pandemic vaccine.
To confirm this hypothesis, we constructed two LAIV strains H2N2 subtype based on the attenuation donor A/Leningrad/134/17/57: A/17/Singapore/57/1 with HA and NA genes from Sing-α2,3 virus (designated as 17/Sing-α2,3) and A/17/Singapore/57/2 with HA and NA genes from Sing-α2,6 virus (17/Sing-α2,6) by reverse genetics methods. HA assay with different RBC confirmed the receptor specificity of the resulting vaccine viruses, which matched that of the corresponding wild-type virus (Fig. 4, a), further indicating the key role of hemagglutinin in binding to host cell glycan receptors. Importantly, adaptation of the vaccine strains to MDCK cells did not result in new mutations in the HA molecule: more than 50 viruses isolated from the plaques matched to the original strain of LAIV. Evaluation of the infectious activity of the engineered viruses showed that the vaccine strains 17/Sing-α2,3 and 17/Sing-α2,6 multiplied equally well in MDCK cells, whereas in eggs, the 17/Sing-α2,3 virus had an infectious titer an order higher than that of the 17/Sing-α2,6 virus (Fig. 4, b).
Fig. 4. Characterization of the investigated vaccine strains of H2N2 LIV in vitro.
a — virus titers in HA assays with untreated chicken erythrocytes (1), horse erythrocytes (2), chicken erythrocytes treated with exosialidase (3); b — infectious activity of the studied viruses in the Egg system and MDCK cell culture.
Twofold immunization of Syrian hamsters with reverse-genetic vaccine strains 17/Sing-α2,3 and 17/Sing-α2,6 resulted in similar levels of serum IgG antibodies, binding to the Sing-α2,3 antigen, with the 17/Sing-α2,3 vaccine virus inducing significantly more antibodies to the Sing-α2,6 antigen than to its own Sing-α2,3 antigen (Fig. 5). The results obtained are in full compliance with the results of studying the antigenicity of pandemic variants of A/Singapore/1/57 in an experiment on mice (Fig. 3).
Fig. 5. Evaluation of the humoral immune response to twice-daily administration of the tested vaccine strains of LIV to Syrian hamsters.
On the left are OD450 values at different dilutions of sera or washes from URT and bronchoalveolar lavage to Sing-α2,3 virus in ELISA. In the middle are OD450 values at different dilutions of sera or washes to Sing-α2,6 virus in ELISA. On the right are the area under the optical density curve at 450 nm in ELISA with the corresponding antigen.
The cross-reactivity of local IgA antibodies in washes from the upper and lower respiratory tracts in ELISA with the same viral antigens was investigated. Using the Sing-α2,6 virus as an antigen revealed significantly higher levels of secretory virus-specific antibodies compared with the use of Sing-α2,3 virus as an antigen (Fig. 5).
Thus, it follows from the results presented that H2N2 subtype influenza viruses with α2-3-receptor specificity induce antibodies with broader cross-reactivity against viruses with different receptor specificity compared with antibodies induced by viruses with affinity for α2-6-receptors. This phenomenon should be taken into account when selecting a strain for vaccine preparation in the event of the onset of an H2N2 influenza pandemic.
Discussion
Influenza A(H2N2) viruses circulated in the human population from 1957 to 1968, after which they were replaced by A(H3N2) viruses that caused the Hong Kong influenza pandemic [18]. Since H2N2 viruses have not infected humans for more than 50 years, population immunity to these viruses is extremely low, and people born after 1968 are the most vulnerable group if H2N2 viruses return to circulation [19]. Given the persistence of influenza viruses with hemagglutinin H2 in the natural reservoir [20–22], the probability of a new H2N2 influenza pandemic is estimated to be high [7]. In this regard, research aimed at the development and detailed study of potentially pandemic vaccines against viruses of this subtype is an urgent and important area.
We have previously developed and researched in preclinical and clinical studies an LAIV against the H2N2 virus circulating at the end of the pandemic wave, A/California/1/66 (H2N2) [23, 24], and this vaccine can be used to immunize the most vulnerable populations in case antigenically similar H2N2 viruses return to circulation. However, results of avian influenza virus monitoring show that most H2N2 subtype isolates remain antigenically similar to the pandemic A/Singapore/1/57 virus and retain a preference for avian-type sialic α2,3 receptors [7]. Detailed studies on the effect of receptor specificity of viruses on their transmissibility in ferret experiments have shown that switching the receptor from α2,3- to α2,6-type significantly increases the ability of the virus transmission by airborne droplets, which may play a crucial role in the pandemic spread of H2N2 viruses [25]. However, there is no clear data on virus strain is best used for vaccine preparation at the onset of a pandemic caused by avian influenza viruses with affinity for both types of cellular receptors.
In the present study, we performed a model experiment with pandemic variants of the A/Singapore/1/57 virus that circulated in 1957 and differed in the receptor specificity of the HA molecule, which was determined by 3 amino acid differences in the HA1 subunit: E156, Q226, G228 for the Sing-α2,3 variant and K156, L226, S228 for the Sing-α2,6 variant. Since it is advisable to produce pandemic vaccines on mammalian cell lines to improve the quality of the product and the possibility of accelerated scaling of production [11, 26], we performed serial passaging of both the original pandemic viruses Sing-α2,3 and Sing-α2,6 and reassortant vaccine strains of LAIV prepared on their basis in MDCK cells, followed by identification of new substitutions in the HA molecule. Interestingly, adaptation mutations occurred in passages in cells of only pandemic viruses, but not vaccine strains of LAIV. This may be due to the fact, that the pandemic variants represented a heterogeneous virus population with an unknown passage history, whereas the reverse-genetic vaccine viruses underwent only two passages in eggs after assembly from plasmids and represented a more homogeneous population. It is important to note that the mutations we found did not affect the receptor specificity of the viruses, but did affect their antigenicity. In particular, the P221S mutation in the HA1 subunit had the character of an escape mutation, as it avoided recognition by antibodies in the sera of animals immunized with all A/Singapore/1/57 variants studied. Interestingly, a similar mutation has been described for avian influenza viruses of the H9N2 subtype, whereby it reduced the affinity of the virus for the avian α2,3-receptor analog, but in combination with the L226Q mutation, the affinity for this receptor was restored [27], which is in complete compliance with our results. Furthermore, the P221S mutation was detected in the A/Wyoming/3/2003 (H3N2) virus during its serial passaging in MDCK cells [28], which also confirms the adaptive nature of this substitution.
Conclusion
The most important result of the study is the demonstration of broader cross-reactivity of antibodies produced by intranasal immunization of animals with H2N2 viruses with α2,3-receptor specificity. This was shown both for pandemic A/Singapore/1/57 viruses and for vaccine reassortant strains of H2N2 obtained by reverse genetics. It is important to note here that the vaccine strain 17/Sing-α2,3 is suitable for cell culture production because it achieves a high infectious titer in MDCK cells, and the homogeneous nature of the strain due to its preparation by genetic engineering methods will ensure the genetic stability of the vaccine during serial passages on MDCK cells, which evidences in favor of mass production of the vaccine in the first wave of the pandemic. Furthermore, this choice of strain for the production of pandemic cell-derived LAIV will maximize the reproduction of the vaccine strain in MDCK cells, as well as ensure high vaccine efficacy due to full antigenic coverage of circulating influenza viruses in the case of a pandemic.
Although our hypothesis has been experimentally confirmed in various animal models, the assessment of immunogenicity and cross-reactivity of the 17/Sing-α2,3 LAIV strain in clinical trials is required for its potential widespread use in humans. One of the obstacles to the use of the 17/Sing-α2,3 strain of LAIV in clinical practice may be the potentially reduced replicative activity of the virus in the human respiratory tract, since in humans α2,3 receptors are poorly represented in the respiratory tract and are predominantly expressed in the lower respiratory tract [29], where the vaccine virus does not replicate due to its temperature-sensitive phenotype, and this may result in low immunogenicity of LAIV. However, experience with human immunization with LAIV against avian influenza H5N1, the infectious agent of which also has α2,3-receptor specificity, has shown that even in the absence of replication in the URT and at low levels of serum antibodies to the virus after intranasal immunization, LAIV produces a long-term immune response that can be de-masked by administration of inactivated influenza vaccine several months or even years later [30, 31]. Accordingly, the strategy of heterologous prime-boost immunization at the beginning of the H2N2 influenza pandemic can also be considered as the most promising for the formation of a powerful long-term humoral immunity with a broad spectrum of protection.
1 WHO. Manual for the laboratory diagnosis of virological surveillance of influenza. Geneva;2011. URL: https://www.who.int/publications/i/item/manual-for-the-laboratory-diagnosis-and-virological-surveillance-of-influenza
2 WHO. Manual for the laboratory diagnosis of virological surveillance of influenza. Geneva;2011. URL: https://www.who.int/publications/i/item/manual-for-the-laboratory-diagnosis-and-virological-surveillance-of-influenza
About the authors
Victoria A. Matyushenko
Institute of Experimental Medicine
Author for correspondence.
Email: matyshenko@iemspb.ru
ORCID iD: 0000-0002-4698-6085
researcher, Laboratory of immunology and vaccine prevention of viral infections, Department of virology named after A.A. Smorodintsev
Russian Federation, St. PetersburgArina D. Kostromitina
Institute of Experimental Medicine
Email: arina8goshina@gmail.com
ORCID iD: 0000-0001-5432-0171
junior researcher, Laboratory of cellular immunology, Department of immunology
Russian Federation, St. PetersburgLarisa G. Rudenko
Institute of Experimental Medicine
Email: vaccine@mail.ru
ORCID iD: 0000-0002-0107-9959
MD, PhD, Professor, Head of the Department of virology named after A.A. Smorodintsev
Russian Federation, St. PetersburgIrina N. Isakova-Sivak
Institute of Experimental Medicine
Email: isakova.sivak@iemspb.ru
ORCID iD: 0000-0002-2801-1508
Dr. Sci. (Biol.), Corresponding Member of the Russian Academy of Sciences, Head, Laboratory of immunology and vaccine prevention of viral infections, Department of virology named after A.A. Smorodintsev
Russian Federation, St. PetersburgReferences
- Charostad J., Rezaei Zadeh Rukerd M., Mahmoudvand S., et al. A comprehensive review of highly pathogenic avian influenza (HPAI) H5N1: An imminent threat at doorstep. Travel Med. Infect. Dis. 2023;55:102638. DOI: https://doi.org/10.1016/j.tmaid.2023.102638
- Tanner W.D., Toth D.J., Gundlapalli A.V. The pandemic potential of avian influenza A(H7N9) virus: a review. Epidemiol. Infect. 2015;143(16):3359–74. DOI: https://doi.org/10.1017/s0950268815001570
- Chen H., Yuan H., Gao R., et al. Clinical and epidemiological characteristics of a fatal case of avian influenza A H10N8 virus infection: a descriptive study. Lancet. 2014;383(9918):714–21. DOI: https://doi.org/10.1016/s0140-6736(14)60111-2
- Yang Z.F., Mok C.K., Peiris J.S., Zhong N.S. Human infection with a novel avian influenza A(H5N6) virus. N. Engl. J. Med. 2015;373(5):487–9. DOI: https://doi.org/10.1056/nejmc1502983
- Connor R.J., Kawaoka Y., Webster R.G., Paulson J.C. Receptor specificity in human, avian, and equine H2 and H3 influenza virus isolates. Virology. 1994;205(1):17–23. DOI: https://doi.org/10.1006/viro.1994.1615
- Matrosovich M., Tuzikov A., Bovin N., et al. Early alterations of the receptor-binding properties of H1, H2, and H3 avian influenza virus hemagglutinins after their introduction into mammals. J. Virol. 2000;74(18):8502–12. DOI: https://doi.org/10.1128/jvi.74.18.8502-8512.2000
- Jones J.C., Baranovich T., Marathe B.M., et al. Risk assessment of H2N2 influenza viruses from the avian reservoir. J. Virol. 2014;88(2):1175–88. DOI: https://doi.org/10.1128/jvi.02526-13
- Nabel G.J., Wei C.J., Ledgerwood J.E. Vaccinate for the next H2N2 pandemic now. Nature. 2011;471(7337):157–8. DOI: https://doi.org/10.1038/471157a
- Rudenko L., Isakova-Sivak I. Pandemic preparedness with live attenuated influenza vaccines based on A/Leningrad/134/17/57 master donor virus. Expert Rev. Vaccines. 2015;14(3):395–412. DOI: https://doi.org/10.1586/14760584.2015.979159
- Chen G.L., Subbarao K. Live attenuated vaccines for pandemic influenza. Curr. Top. Microbiol. Immunol. 2009;333:109–32. DOI: https://doi.org/10.1007/978-3-540-92165-3_5
- Hegde N.R. Cell culture-based influenza vaccines: a necessary and indispensable investment for the future. Hum. Vaccin. Immunother. 2015;11(5):1223–34. DOI: https://doi.org/10.1080/21645515.2015.1016666
- Hussain A.I., Cordeiro M., Sevilla E., Liu J. Comparison of egg and high yielding MDCK cell-derived live attenuated influenza virus for commercial production of trivalent influenza vaccine: in vitro cell susceptibility and influenza virus replication kinetics in permissive and semi-permissive cells. Vaccine. 2010;28(22):3848–55. DOI: https://doi.org/10.1016/j.vaccine.2010.03.005
- Liu J., Shi X., Schwartz R., Kemble G. Use of MDCK cells for production of live attenuated influenza vaccine. Vaccine. 2009;27(46):6460–3. DOI: https://doi.org/10.1016/j.vaccine.2009.06.024
- Киселева И.В., Исакова И.Н., Ларионова Н.В. и др. Эффективность получения реассортантов между эпидемическими и холодоадаптированнымн вирусами гриппа в развивающихся куриных эмбрионах и в культуре клеток MDCK. Журнал микробиологии, эпидемиологии и иммунобиологии. 2007; 84(6):40–5. Kiseleva I.V., Isakova I.N., Larionova N.V., et al. Efficacy of production of reassortants between epidemic and cold-adapted influenza viruses in growing chicken embryos and in MDCK cell culture. Journal of Microbiology, Epidemiology and Immunobiology. 2007;84(6):40–5. EDN: https://elibrary.ru/iisqbx
- Hoffmann E., Neumann G., Kawaoka Y., et al. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl Acad. Sci. USA. 2000;97(11):6108–13. DOI: https://doi.org/10.1073/pnas.100133697
- Isakova-Sivak I., Chen L.M., Matsuoka Y., et al. Genetic bases of the temperature-sensitive phenotype of a master donor virus used in live attenuated influenza vaccines: A/Leningrad/134/17/57 (H2N2). Virology. 2011;412(2):297–305. DOI: https://doi.org/10.1016/j.virol.2011.01.004
- Reed L.J., Muench H. A simple method of estimating fifty per cent endpoints. Am. J. Epidemiol. 1938;27(3):493–7.
- Kilbourne E.D. Influenza pandemics of the 20th century. Emerg. Infect. Dis. 2006;12(1):9–14. DOI: https://doi.org/10.3201/eid1201.051254
- Babu T.M., Perera R.A.P.M., Wu J.T., et al. Population serologic immunity to human and avian H2N2 viruses in the United States and Hong Kong for pandemic risk assessment. J. Infect. Dis. 2018;218(7):1054–60. DOI: https://doi.org/10.1093/infdis/jiy291
- Ma W., Vincent A.L., Gramer M.R., et al. Identification of H2N3 influenza A viruses from swine in the United States. Proc. Natl Acad. Sci. USA. 2007;104(52):20949–54. DOI: https://doi.org/10.1073/pnas.0710286104
- Schäfer J., Khristova M.L., Busse T.L., et al. Analysis of internal proteins of influenza A (H2N2) viruses isolated from birds in East Germany in 1983. Acta Virol. 1992;36(2):113–20.
- Makarova N.V., Kaverin N.V., Krauss S., et al. Transmission of Eurasian avian H2 influenza virus to shorebirds in North America. J. Gen. Virol. 1999;80(Pt. 12):3167–71. DOI: https://doi.org/10.1099/0022-1317-80-12-3167
- Isakova-Sivak I., de Jonge J., Smolonogina T., et al. Development and pre-clinical evaluation of two LAIV strains against potentially pandemic H2N2 influenza virus. PloS One. 2014;9(7):e102339. DOI: https://doi.org/10.1371/journal.pone.0102339
- Isakova-Sivak I., Stukova M., Erofeeva M., et al. H2N2 live attenuated influenza vaccine is safe and immunogenic for healthy adult volunteers. Hum. Vaccin. Immunother. 2015;11(4):970–82. DOI: https://doi.org/10.1080/21645515.2015.1010859
- Pappas C., Viswanathan K., Chandrasekaran A., et al. Receptor specificity and transmission of H2N2 subtype viruses isolated from the pandemic of 1957. PloS One. 2010;5(6):e11158. DOI: https://doi.org/10.1371/journal.pone.0011158
- Genzel Y., Reichl U. Continuous cell lines as a production system for influenza vaccines. Expert Rev. Vaccines. 2009;8(12): 1681–92. DOI: https://doi.org/10.1586/erv.09.128
- An S.H., Son S.E., Song J.H., et al. Selection of an optimal recombinant Egyptian H9N2 avian influenza vaccine strain for poultry with high antigenicity and safety. Vaccines (Basel). 2022;10(2):162. DOI: https://doi.org/10.3390/vaccines10020162
- Barnard K.N., Wasik B.R., Alford B.K., et al. Sequence dynamics of three influenza A virus strains grown in different MDCK cell lines, including those expressing different sialic acid receptors. J. Evol. Biol. 2021;34(12):1878–900. DOI: https://doi.org/10.1111/jeb.13890
- de Graaf M., Fouchier R.A. Role of receptor binding specificity in influenza A virus transmission and pathogenesis. EMBO J. 2014;33(8):823–41. DOI: https://doi.org/10.1002/embj.201387442
- Rudenko L., Naykhin A., Donina S., et al. Assessment of immune responses to H5N1 inactivated influenza vaccine among individuals previously primed with H5N2 live attenuated influenza vaccine. Hum. Vaccin. Immunother. 2015; 11(12): 2839–48. DOI: https://doi.org/10.1080/21645515.2015.1069931
- Talaat K.R., Luke C.J., Khurana S., et al. A live attenuated influenza A(H5N1) vaccine induces long-term immunity in the absence of a primary antibody response. J. Infect. Dis. 2014;209(12):1860–9. DOI: https://doi.org/10.1093/infdis/jiu123
Supplementary files