Analysis of influenza epidemics during the COVID-19 pandemic using an improved surveillance system (from 2021 to 2024)
- Authors: Karpova L.S.1, Pelikh M.Y.1, Stolyarov K.A.1, Volik K.M.1, Stolyarova T.P.1, Danilenko D.M.1
-
Affiliations:
- Smorodintsev Research Institute of Influenza
- Issue: Vol 101, No 5 (2024)
- Pages: 679-691
- Section: ORIGINAL RESEARCHES
- URL: https://microbiol.crie.ru/jour/article/view/18689
- DOI: https://doi.org/10.36233/0372-9311-556
- EDN: https://elibrary.ru/tqkwng
- ID: 18689
Cite item
Abstract
Aim. Assessing the effectiveness of new baselines and intensity thresholds of epidemics based on rates of incidence and hospitalization with a diagnosis of “influenza” to clarify the timing of epidemics and their spread throughout the Russian Federation against the backdrop of the COVID-19 pandemic (from 2021 to 2024).
Materials and methods. At the A.A. Smorodintsev Influenza Research Institute, the software was reformed taking into account the need to solve the tasks set during the COVID-19 pandemic. Due to changes in influenza surveillance in relation to the diagnosis of “influenza”, and hence the increase in the registration of influenza cases, the baseline and threshold of epidemics were adjusted for the influenza incidence and hospitalization rates in the surveyed cities in total (61) and for each Federal districts (over the entire population and by age groups) for 3 epidemics against the background of COVID-19 pandemic (2021–2022, 2022–2023, and 2023–2024).
Results. A comparison of baselines calculated over the previous 6 seasons based on the incidence and hospitalization rates of mostly clinically diagnosed influenza and new baseline levels of incidence and hospitalization rates of mostly laboratory-confirmed influenza during the pandemic showed minor changes in the indicators of baseline incidence and hospitalization rates while epidemic thresholds for these indicators increased.
Conclusion. Against the backdrop of the COVID-19 pandemic during the 2020–2021 season, there was no influenza epidemic. In 2021–2022, the A(H3N2) epidemic was of low intensity in terms of incidence, hospitalization rates and low mortality (2 cases). In 2022–2023, the influenza A(H1N1)pdm09 and B epidemic was of moderate intensity in terms of incidence, with a high frequency of hospitalizations and mortality (120 cases). Influenza A(H3N2) and B epidemic in 2023–2024 was of a “very high” level in terms of the influenza incidence, but average in terms of the frequency of hospitalizations and mortality (41 cases), with higher incidence rate compared to the previous epidemic (0.28% and 0.19% of the total population), including persons over 15 years of age (0.19% and 0.12%).
Keywords
Full Text
Introduction
A new coronavirus infection has been circulating in Russia for the last 4 seasons. Against this background, to accurately determine the start of the epidemic in the country, it is necessary to use incidence data only for influenza, without taking into account acute respiratory viral infection (ARVI), because incidence data for ARVI and COVID-19, which significantly outnumber influenza during the pandemic, mask the place, time of the start and nature of the development of the influenza epidemic. Due to the similarity of the clinical course of influenza, COVID-19 and other acute respiratory viruses, according to the Government Decree of December 14, 2022 № 2297, testing for influenza and other acute respiratory viruses in hospitals and polyclinics is carried out within the framework of the program of state guarantees of free medical care for citizens and simultaneously with the polymerase chain reaction (PCR) test for coronavirus1.
The aim of the study is to assess the effectiveness of new base lines and intensity thresholds of epidemics in terms of morbidity and hospitalization with the diagnosis of “influenza” to clarify the timing of epidemics and their spread across Russia against the background of the COVID-19 pandemic (from 2021 to 2024).
Materials and methods
At the A.A. Smorodintsev Influenza Research Institute, the software was reformed taking into account the need to solve the tasks set during the SARS-CoV-2 pandemic. The introduction of a new electronic system, based on the creation of a flexible platform, allowed us to respond quickly by changing or adding electronic forms to the requirements for data collection and analysis and uploading the results to the WHO global database [1].
Previously, we calculated baselines and thresholds of influenza incidence for 6 seasons (from 2016-2017 to 2022-2023) using the moving epidemic method adopted in the European influenza surveillance system [2, 3]. Due to changes in influenza surveillance regarding the diagnosis of influenza and other acute respiratory infections, and hence the increase in influenza case registration, we adjusted the baselines and thresholds of epidemics for influenza incidence and frequency of hospitalizations diagnosed with influenza in the observed cities (61 in total) and for each federal district (FD) (for the whole population and age groups) for 3 epidemics occurring against the background of the COVID-19 pandemic (2021–2022, 2022–2023 and 2023–2024).
Statistical processing of the obtained results was carried out in the MS Excel program using Student’s t-criterion, with significance P = 95%.
Results and discussion
Comparison of baselines calculated over the previous 6 seasons for incidence and hospitalization rates of mostly clinically diagnosed influenza and new baseline incidence and hospitalization rates of mostly laboratory-confirmed influenza during the pandemic showed little change in baseline incidence and hospitalization rates, while epidemic thresholds for these indicators increased (Tables 1, 2).
Table 1. Baselines and thresholds of influenza incidence rate, per 10,000
Parameter | 2016–2017 – 2022–2023 | 2021–2022 – 2023–2024 | |||||||||
total | age, years | total | age, years | ||||||||
0–2 | 3–6 | 7–14 | 15+ | 0–2 | 3–6 | 7–14 | 15+ | ||||
Russia | |||||||||||
BL | pre-epidemic | 0,05 | 0,23 | 0,13 | 0,08 | 0,04 | 0,04 | 0,23 | 0,13 | 0,05 | 0,03 |
post-epidemic | 0,04 | 0,21 | 0,17 | 0,09 | 0,04 | 0,05 | 0,28 | 0,19 | 0,10 | 0,04 | |
IT | medium | 0,36 | 1,32 | 1,40 | 0,72 | 0,21 | 0,92 | 3,87 | 3,84 | 2,60 | 0,40 |
high | 1,12 | 5,39 | 4,38 | 2,35 | 0,65 | 2,95 | 9,83 | 9,28 | 6,91 | 1,92 | |
very high | 1,46 | 7,20 | 5,69 | 3,07 | 0,84 | 3,85 | 12,47 | 11,69 | 8,81 | 2,59 | |
Central Federal District | |||||||||||
L | pre-epidemic | 0,06 | 0,24 | 0,24 | 0,13 | 0,03 | 0,05 | 0,20 | 0,13 | 0,07 | 0,05 |
post-epidemic | 0,03 | 0,12 | 0,12 | 0,05 | 0,02 | 0,05 | 0,11 | 0,16 | 0,08 | 0,02 | |
T | medium | 0,15 | 0,57 | 1,01 | 0,68 | 0,17 | 1,42 | 5,37 | 6,94 | 5,26 | 0,59 |
high | 1,82 | 9,56 | 9,25 | 5,32 | 1,21 | 3,97 | 16,44 | 18,35 | 13,70 | 1,94 | |
very high | 2,56 | 13,54 | 12,89 | 7,38 | 1,67 | 5,10 | 21,33 | 23,39 | 17,42 | 2,54 | |
Southern Federal District | |||||||||||
BL | pre-epidemic | 0,06 | 0,12 | 0,16 | 0,15 | 0,07 | 0,07 | 0,11 | 0,11 | 0,26 | 0,06 |
post-epidemic | 0,06 | 0,25 | 0,17 | 0,08 | 0,06 | 0,06 | 0,34 | 0,14 | 0,16 | 0,06 | |
IT | medium | 0,47 | 1,89 | 1,74 | 0,73 | 0,27 | 0,57 | 3,43 | 2,20 | 0,81 | 0,28 |
high | 1,02 | 5,15 | 3,73 | 1,56 | 0,68 | 2,20 | 7,70 | 6,07 | 4,43 | 1,53 | |
very high | 1,27 | 6,60 | 4,61 | 1,93 | 0,86 | 2,92 | 9,59 | 7,78 | 6,04 | 2,08 | |
Northwest Federal District | |||||||||||
BL | pre-epidemic | 0,03 | 0,16 | 0,17 | 0,07 | 0,02 | 0,03 | 0,16 | 0,15 | 0,03 | 0,02 |
post-epidemic | 0,05 | 0,26 | 0,26 | 0,20 | 0,04 | 0,07 | 0,31 | 0,31 | 0,24 | 0,04 | |
IT | medium | 0,36 | 1,31 | 1,38 | 0,93 | 0,21 | 0,54 | 3,56 | 2,90 | 2,24 | 2,42 |
high | 1,16 | 5,06 | 4,02 | 2,49 | 0,77 | 6,31 | 10,40 | 10,96 | 9,86 | 8,31 | |
very high | 1,51 | 6,72 | 5,18 | 3,17 | 1,02 | 8,85 | 13,43 | 14,53 | 13,22 | 10,91 | |
Far Eastern Federal District | |||||||||||
BL | pre-epidemic | 0,17 | 0,31 | 0,30 | 0,30 | 0,10 | 0,16 | 0,34 | 0,16 | 0,21 | 0,12 |
post-epidemic | 0,11 | 0,66 | 0,60 | 0,24 | 0,08 | 0,11 | 0,83 | 0,70 | 0,30 | 0,10 | |
IT | medium | 0,91 | 3,07 | 2,69 | 1,45 | 0,58 | 1,56 | 6,27 | 5,33 | 3,74 | 0,80 |
high | 2,04 | 8,45 | 6,62 | 4,15 | 1,27 | 3,63 | 14,15 | 11,68 | 7,71 | 2,27 | |
very high | 2,54 | 10,83 | 8,36 | 5,34 | 1,58 | 4,54 | 17,64 | 14,49 | 9,47 | 2,91 | |
Siberian Federal District | |||||||||||
BL | pre-epidemic | 0,02 | 0,09 | 0,09 | 0,03 | 0,01 | 0,02 | 0,09 | 0,08 | 0,03 | 0,01 |
post-epidemic | 0,04 | 0,17 | 0,14 | 0,08 | 0,02 | 0,05 | 0,13 | 0,14 | 0,08 | 0,03 | |
IT | medium | 0,40 | 1,77 | 1,49 | 0,80 | 0,21 | 0,53 | 3,14 | 2,03 | 1,53 | 0,20 |
high | 0,75 | 4,43 | 2,95 | 1,91 | 0,41 | 1,24 | 6,83 | 3,81 | 2,85 | 0,75 | |
very high | 0,90 | 5,60 | 3,59 | 2,40 | 0,50 | 1,55 | 8,47 | 4,60 | 3,43 | 0,99 | |
North Caucasian Federal District | |||||||||||
BL | pre-epidemic | 0,03 | 0,14 | 0,29 | 0,22 | 0,03 | 0,19 | 0,27 | 0,29 | 0,20 | 0,53 |
post-epidemic | 0,04 | 0,14 | 0,39 | 0,11 | 0,04 | 0,06 | 0,49 | 0,23 | 0,27 | 0,04 | |
IT | medium | 0,17 | 2,83 | 2,38 | 0,77 | 0,13 | 0,41 | 6,24 | 4,68 | 3,28 | 1,02 |
high | 2,23 | 7,55 | 7,70 | 6,27 | 1,68 | 3,33 | 10,66 | 10,84 | 10,40 | 3,30 | |
very high | 3,15 | 9,63 | 10,04 | 8,69 | 2,37 | 4,63 | 12,61 | 13,56 | 13,55 | 4,30 | |
Ural Federal District | |||||||||||
BL | pre-epidemic | 0,03 | 0,07 | 0,06 | 0,03 | 0,03 | 0,03 | 0,12 | 0,08 | 0,05 | 0,02 |
post-epidemic | 0,04 | 0,09 | 0,10 | 0,04 | 0,04 | 0,04 | 0,09 | 0,06 | 0,02 | 0,05 | |
IT | medium | 0,23 | 0,24 | 0,33 | 0,28 | 0,24 | 0,26 | 1,02 | 0,65 | 0,51 | 0,35 |
high | 0,59 | 1,26 | 1,10 | 0,71 | 0,60 | 1,23 | 3,13 | 2,70 | 1,74 | 1,17 | |
very high | 0,76 | 1,71 | 1,44 | 0,90 | 0,76 | 1,65 | 4,07 | 3,61 | 2,27 | 1,54 | |
Volga Federal District | |||||||||||
BL | pre-epidemic | 0,02 | 0,12 | 0,10 | 0,03 | 0,02 | 0,01 | 0,14 | 0,08 | 0,02 | 0,01 |
post-epidemic | 0,05 | 0,30 | 0,18 | 0,09 | 0,04 | 0,06 | 0,32 | 0,16 | 0,07 | 0,04 | |
IT | medium | 0,37 | 1,40 | 1,32 | 0,56 | 0,23 | 0,74 | 2,57 | 2,57 | 2,06 | 0,42 |
high | 0,95 | 3,53 | 2,76 | 2,08 | 0,67 | 2,68 | 10,73 | 7,75 | 5,24 | 1,87 | |
very high | 1,21 | 4,48 | 3,40 | 2,75 | 0,86 | 3,54 | 14,34 | 10,03 | 6,65 | 2,51 | |
Table 2. Baselines and thresholds for rates of hospitalization with “influenza”, per 10,000
Parameter | 2016–2017 – 2022–2023 | 2021–2022 – 2023–2024 | |||||||||
total | age, years | total | age, years | ||||||||
0–2 | 3–6 | 7–14 | 15+ | 0–2 | 3–6 | 7–14 | 15+ | ||||
Russia | |||||||||||
BL | pre-epidemic | 0,03 | 0,15 | 0,09 | 0,05 | 0,03 | 0,01 | 0,11 | 0,04 | 0,02 | 0,01 |
post-epidemic | 0,03 | 0,14 | 0,11 | 0,06 | 0,03 | 0,02 | 0,25 | 0,07 | 0,03 | 0,01 | |
IT | medium | 0,24 | 1,13 | 0,91 | 0,42 | 0,14 | 0,27 | 1,92 | 1,18 | 0,55 | 0,13 |
high | 0,49 | 3,04 | 1,86 | 0,80 | 0,29 | 0,62 | 4,24 | 2,35 | 1,01 | 0,35 | |
very high | 0,60 | 3,89 | 2,28 | 0,97 | 0,35 | 0,77 | 5,26 | 2,87 | 1,22 | 0,45 | |
Central Federal District | |||||||||||
BL | pre-epidemic | 0,04 | 0,19 | 0,19 | 0,08 | 0,02 | 0,01 | 0,13 | 0,07 | 0,03 | 0,01 |
post-epidemic | 0,02 | 0,09 | 0,07 | 0,03 | 0,01 | 0,02 | 0,10 | 0,08 | 0,05 | 0,01 | |
IT | medium | 0,15 | 0,78 | 0,81 | 0,40 | 0,10 | 0,30 | 2,12 | 1,69 | 0,74 | 0,11 |
high | 0,45 | 3,82 | 2,67 | 1,03 | 0,23 | 0,69 | 5,59 | 3,79 | 1,41 | 0,30 | |
very high | 0,58 | 5,16 | 3,49 | 1,31 | 0,29 | 0,86 | 7,12 | 4,71 | 1,71 | 0,39 | |
Southern Federal District | |||||||||||
BL | pre-epidemic | 0,06 | 0,11 | 0,15 | 0,14 | 0,06 | 0,06 | 0,10 | 0,11 | 0,08 | 0,03 |
post-epidemic | 0,05 | 0,21 | 0,72 | 0,07 | 0,04 | 0,05 | 0,25 | 0,11 | 0,13 | 0,05 | |
IT | medium | 0,45 | 1,93 | 1,71 | 0,68 | 0,24 | 0,47 | 3,32 | 1,95 | 0,83 | 0,20 |
high | 0,96 | 5,09 | 3,69 | 1,52 | 0,60 | 1,00 | 6,22 | 3,01 | 1,52 | 0,65 | |
very high | 1,18 | 6,49 | 4,57 | 1,89 | 0,76 | 1,24 | 7,51 | 3,47 | 1,82 | 0,84 | |
Northwest Federal District | |||||||||||
BL | pre-epidemic | 0,02 | 0,20 | 0,15 | 0,06 | 0,01 | 0,03 | 0,23 | 0,16 | 0,07 | 0,02 |
post-epidemic | 0,03 | 0,19 | 0,18 | 0,17 | 0,03 | 0,04 | 0,17 | 0,16 | 0,09 | 0,02 | |
IT | medium | 0,24 | 1,21 | 0,94 | 0,56 | 0,13 | 0,33 | 1,91 | 1,21 | 0,78 | 0,37 |
high | 0,71 | 3,82 | 2,32 | 1,29 | 0,46 | 0,92 | 5,08 | 2,93 | 1,67 | 0,77 | |
very high | 0,91 | 4,97 | 2,93 | 1,62 | 0,60 | 1,18 | 6,48 | 3,70 | 2,06 | 0,94 | |
Parameter | 2016–2017 – 2022–2023 | 2021–2022 – 2023–2024 | |||||||||
total | age, years | total | age, years | ||||||||
0–2 | 3–6 | 7–14 | 15+ | 0–2 | 3–6 | 7–14 | 15+ | ||||
Far Eastern Federal District | |||||||||||
BL | pre-epidemic | 0,13 | 0,23 | 0,23 | 0,24 | 0,09 | 0,00 | 0,08 | 0,14 | 0,12 | 0,07 |
post-epidemic | 0,08 | 0,41 | 0,36 | 0,12 | 0,06 | 0,07 | 0,74 | 0,19 | 0,22 | 0,08 | |
IT | medium | 0,62 | 2,40 | 1,62 | 0,87 | 0,42 | 0,62 | 3,50 | 1,70 | 0,92 | 0,38 |
high | 1,28 | 6,20 | 3,70 | 1,80 | 0,86 | 1,43 | 7,75 | 4,10 | 2,02 | 0,95 | |
very high | 1,57 | 7,88 | 4,61 | 2,21 | 1,05 | 1,79 | 9,63 | 5,15 | 2,51 | 1,20 | |
Siberian Federal District | |||||||||||
BL | pre-epidemic | 0,02 | 0,08 | 0,07 | 0,03 | 0,01 | 0,01 | 0,13 | 0,03 | 0,03 | 0,00 |
post-epidemic | 0,02 | 0,14 | 0,11 | 0,06 | 0,01 | 0,02 | 0,08 | 0,07 | 0,03 | 0,01 | |
IT | medium | 0,21 | 1,33 | 0,81 | 0,36 | 0,09 | 0,22 | 2,26 | 0,79 | 0,38 | 0,07 |
high | 0,43 | 3,31 | 1,65 | 0,73 | 0,22 | 0,46 | 4,50 | 1,68 | 0,58 | 0,23 | |
very high | 0,53 | 4,19 | 2,03 | 0,89 | 0,28 | 0,57 | 5,48 | 2,08 | 0,66 | 0,30 | |
North Caucasian Federal District | |||||||||||
BL | pre-epidemic | 0,01 | 0,00 | 0,18 | 0,17 | 0,02 | 0,00 | 0,00 | 0,00 | 0,14 | 0,00 |
post-epidemic | 0,02 | 0,14 | 0,25 | 0,06 | 0,03 | 0,01 | 0,35 | 0,00 | 0,00 | 0,00 | |
IT | medium | 0,15 | 2,00 | 1,42 | 0,74 | 0,10 | 0,08 | 3,29 | 1,48 | 1,44 | 0,15 |
high | 0,67 | 4,46 | 3,39 | 1,67 | 0,45 | 0,70 | 5,12 | 3,93 | 2,18 | 0,56 | |
very high | 0,91 | 5,54 | 4,26 | 2,08 | 0,60 | 0,98 | 5,94 | 5,01 | 2,51 | 0,75 | |
Ural Federal District | |||||||||||
BL | pre-epidemic | 0,01 | 0,06 | 0,05 | 0,02 | 0,02 | 0,00 | 0,05 | 0,04 | 0,02 | 0,00 |
post-epidemic | 0,02 | 0,08 | 0,03 | 0,00 | 0,03 | 0,03 | 0,00 | 0,00 | 0,00 | 0,01 | |
IT | medium | 0,11 | 0,21 | 0,16 | 0,06 | 0,14 | 0,07 | 0,49 | 0,29 | 0,04 | 0,09 |
high | 0,27 | 0,82 | 0,46 | 0,22 | 0,30 | 0,26 | 3,32 | 0,91 | 0,45 | 0,20 | |
very high | 0,34 | 1,09 | 0,59 | 0,29 | 0,37 | 0,34 | 4,57 | 1,18 | 0,62 | 0,25 | |
Volga Federal District | |||||||||||
BL | pre-epidemic | 0,02 | 0,12 | 0,10 | 0,03 | 0,02 | 0,01 | 0,08 | 0,06 | 0,01 | 0,01 |
post-epidemic | 0,03 | 0,23 | 0,14 | 0,08 | 0,02 | 0,02 | 0,15 | 0,04 | 0,02 | 0,01 | |
IT | medium | 0,24 | 1,05 | 0,76 | 0,32 | 0,16 | 0,22 | 1,38 | 0,70 | 0,31 | 0,15 |
high | 0,44 | 2,50 | 1,58 | 0,67 | 0,28 | 0,57 | 4,26 | 1,89 | 0,86 | 0,35 | |
very high | 0,53 | 3,15 | 1,94 | 0,83 | 0,34 | 0,72 | 5,53 | 2,41 | 1,11 | 0,45 | |
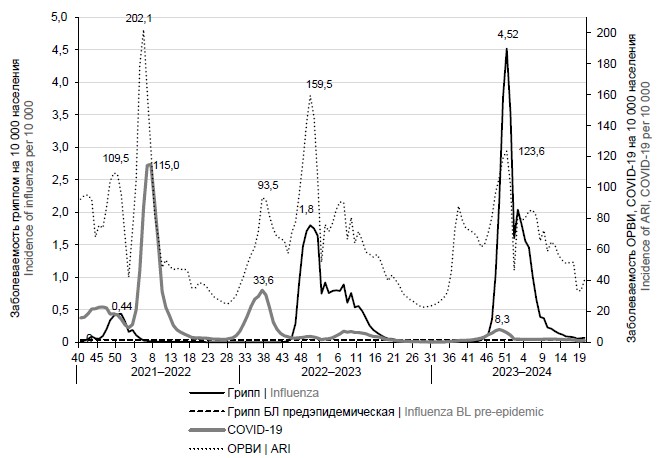
Monitoring for influenza incidence in the country during the 2023–2024 season showed its early increase: as early as week 45 of 2023 (2nd week of November), it exceeded the baseline (0.04 per 10,000 population) by 87.5% nationwide. Further, there was a steady increase in influenza incidence for 6 weeks with a peak (4.52 per 10,000 population) in week 51 of 2023. From the following week, the incidence began to decline but remained at a low level until week 18. The incidence rate at the peak of the epidemic (2023–2024) was 2.5 times higher than the 2022–2023 epidemic. The intensity of the last season’s influenza epidemic was very high, while in the previous epidemic it was intermediate (Fig. 1).
Fig. 1. Dynamics of influenza incidence in the population of the surveyed cities (61) in the seasons 2021–2022, 2022–2023, and 2023–2024.
Monitoring the incidence in different age groups of the population
In the 2023–2024 influenza season, influenza incidence exceeded the baseline in week 45 simultaneously in all age groups. Peak incidence was recorded in week 51 simultaneously in pediatric age groups and among persons over 15 years of age. The intensity of influenza incidence at the peak of the epidemic exceeded the very high intensity threshold in all age groups except children 0–2 years of age, in whom it was high. From week 52 onwards, incidence began to decline in all age groups, but remained above post-epidemic baseline in children 0–2 and 3–6 years of age until week 15 (inclusive), and among children 7–14 years of age and persons 15+ years of age until week 18.
During the 2023–2024 epidemic period, 0.27% of the total population of the observed cities (150,439 persons) became ill with influenza, including 0.88% of children aged 0–2 years, 0.8% of children aged 3–6 years, 0.57% of children aged 7–14 years, and 0.19% of persons aged 15 years and older. During the 2022–2023 epidemic period, 0.19% of the total population of the monitored cities (105,881 persons) became ill with influenza, including 0.81% of children aged 0–2 years, 0.66% of children aged 3–6 years, 0.46% of children aged 7–14 years, and 0.12% of persons aged 15 years and older (Fig. 2).
Fig. 2. Dynamics of influenza incidence in different age groups of the population of the surveyed cities (61) in the 2023–2024 season.
Geographical spread of the epidemic, its intensity in different Federal Districts
The epidemic started first of all (week 43) in the cities of the Urals Federal District; in week 44 it was registered in the other 3 Federal Districts (North-Western, Volga and Central), in week 46 in the Siberian Federal District, in week 47 in the Far Eastern Federal District, in week 49 in the Southern Federal District, and last of all in the North Caucasus Federal District (week 51).
The peak incidence was reached earliest (week 50) in the Far Eastern Federal District (4.6 per 10,000 population), in week 51 in the Northwestern (11.56), Central (5.41) and Ural Federal Districts (1.91), in week 52 in the Siberian Federal District (1.59), in week 2 in the Volga Federal District (3.57), and in week 5 in the North Caucasus (4.94) and Southern Federal Districts (3.86). The influenza epidemic ended earliest (at week 13) in the Siberian and Far Eastern FDs, at week 14 in the Volga and North Caucasus FDs, at week 17 in the Southern FD, and at week 19 in the Central FD; however, in the Northwestern and Ural FDs, influenza incidence remained above their post-epidemic baselines at week 19. Thus, the duration of the epidemic in the districts varied from 16 weeks in the North Caucasus FD to 29 weeks in the Urals FD.
Incidence intensity at the peak of the epidemic
The intensity of influenza incidence at the peak of the epidemic was very high, far exceeding the threshold of this level, in the Northwestern FD (11.6 vs. 8.85 per 10,000 of the population) and Southern FD (3.9 vs. 2.92 per 10,000 of the population); in the other FDs it also reached a fairly high level but only slightly exceeded this threshold (Fig. 3).
Fig. 3. Comparison of the dynamics and intensity level of influenza incidence in different Federal Districts (FD) in the 2023–2024 season.
Hospitalization rates
An increase in the frequency of influenza hospitalizations led to the exceeding of the BL at week 45, at the same time as the onset of the upsurge. Hospitalization peaked (0.55 per 10,000 of the population) at week 51, when it exceeded the medium intensity threshold. Thereafter, hospitalization rates declined and were low intensity from week 6 and below baseline from week 15 (Fig. 4). The decrease in hospitalization rates from March to May is apparently explained by the predominant circulation of influenza B virus at this time and a milder course of the disease than in influenza A(H3N2).
Fig. 4. Dynamics of the frequency of hospitalization of patients diagnosed with influenza in seasons 2021–2022, 2022–2023, and 2023–2024.
During the epidemic period, 0.05% of the total population was hospitalized, including 0.32% of children aged 0-2 years, 0.16% of children aged 3–6 years, 0.07% of children aged 7–14 years, and 0.02% of persons aged 15–64 years and 0.05% of persons over 65 years. The proportion of persons hospitalized during the epidemic period from the number of influenza cases averaged about 17.3%, including 35.9% among children aged 0–2 years, 19.6% among 3–6 years, 12.6% among 7–14 years, 12.7% among persons aged 15–64 years, and 26.7% among persons over 65 years old.
Influenza martality rates
In the 2023-2024 season, 41 deaths from laboratory-confirmed influenza were reported: 39 cases of influenza A(H3N2) and 2 cases of influenza A(H3N2)+COVID-19. This season, deaths were recorded from week 47 of 2023 through week 15 of 2024 (November through April) and only from influenza A(H3N2), i.e., during its circulation period. Deaths from mixed A(H3N2) and COVID-19 infection were reported in January and April. There were no deaths from influenza B, despite its predominant circulation from March to May.
During the previous epidemic in the 2022–2023 season, when influenza A(H1N1)pdm09 was the main causative agent, 120 influenza-related deaths were laboratory-confirmed: 103 from influenza A(H1N1)pdm09, 6 from influenza B, 1 from influenza A(H3N2) and 10 from influenza A (not subtyped).
It should be noted that in the 2021–2022 epidemic, where only influenza A(H3N2) virus was the pathogen, only 2 deaths from laboratory-confirmed influenza were reported (Fig. 5).
Fig. 5. The number and etiology of deaths from laboratory-confirmed influenza in the epidemic from 2021 to 2024.
The age structure of those who died in the last season was dominated by elderly people aged 65+ years (56.1%; p < 0.05). The proportion of the deceased aged 42–64 years was 24.3%, the proportion of children under 6 years of age was 4.8%, and 7–14 years of age was 4.8% of the total number of the dead (Fig. 6). Patients with cardiovascular disease accounted for 66.0% (p < 0.05) and internal diseases for 44.0% (p < 0.05) of the deaths, which is associated with an increase in the elderly during the last epidemic. Other risk factors for fatal outcomes were such comorbidities as chronic lung diseases (17.1%) and immunodeficiency conditions (17.1%).
Fig. 6. Age structure and structure of background pathology of those who died from laboratory confirmed influenza during the epidemic in 2021–2024.
1 — obesity; 2 — diabetes; 3 — immunodeficiencies; 4 — diseases of internal organs; 5 — cardiovascular pathology; 6 — chronic lung diseases; 7 — diseases of the central nervous system; 8 — pregnancy.
Comparison of influenza, ARVI and COVID-19 incidence dynamics showed alternation of influenza and COVID-19 pathogens (Fig. 7). In the 2021–2022 season, the Delta genetic variant wave preceded a low-intensity influenza A(H3N2) epidemic, which in turn was succeeded by a high-intensity Omicron genetic variant epidemic. In the 2022–2023 season, the epidemic caused by the daughter Omicron genetic variants was replaced by an influenza A(H1N1)pdm09 and B epidemic of medium intensity in terms of incidence. It was not until the 2023–2024 season that the COVID-19 wave and the A(H3N2) and B epidemics began simultaneously, with the COVID-19 wave being of low intensity and the influenza A(H3N2) and B epidemics being of very high intensity.
Fig. 7. Comparison of the incidence dynamics of influenza, ARVI and COVID-19 in the surveyed cities during the seasons from 2021 to 2024.
Other researchers provide data indicating possible interference of SARS-CoV-2, influenza and other ARVI pathogens with each other according to both sentinel and traditional surveillance data [4–6].
The peculiarity of the 2023–2024 influenza epidemic was an early onset (in week 45 of 2023), as in other influenza epidemics against the background of COVID-19 circulation (in 2021 — in week 45, in 2022 — in week 47). Early onset of influenza epidemics during COVID-19 circulation was also noted in Belarus; the influenza epidemic season of 2021–2022 and 2023–2024 started from week 47, and in Tashkent, the influenza epidemic season of 2023–2024 started from week 44 [7-9].
Such an early onset of influenza epidemics has been observed only in the history of influenza pandemics: influenza pandemic A/Singapore/57(H2N2) began in the 39th calendar week of 1957, pandemic A/USSR/90/77(H1N1) began in November 1977, and pandemic A/California/09(H1N1) began in the 39th calendar week of 2009 [10–14].
It can be assumed that the early onset of influenza pandemics could be due to antigenic novelty of the pandemic influenza viruses, A/Singapore/57(H2N2), A/California/09(H1N1), to which the majority of the population was not immune, and, during the COVID-19 pandemic, due to decreased immunity to influenza in the population that had previously been infected with COVID-19.
Conclusion
Comparison of baselines calculated for 6 seasons before the COVID-19 pandemic and new BLs and PIs of epidemics in terms of incidence and PCR-confirmed influenza hospitalizations calculated for 3 epidemics against the background of the COVID-19 pandemic showed little change in baselines, while the intensity thresholds increased.
There was no influenza epidemic in the background of COVID-19 pandemic in the first season (2020–2021). In the 2021–2022 season, the A(H3N2) monoethiology epidemic was of low intensity in terms of morbidity and hospitalization rate, as well as low mortality (2 cases). In the 2022–2023 season, the influenza A(H1N1)pdm09 and B epidemic was of medium intensity in terms of incidence, with a high incidence of hospitalizations and high lethality (120 cases). The influenza A(H3N2) and B epidemic in the 2023–2024 season was of very high intensity in terms of influenza incidence, but medium in terms of hospitalization rate and mortality (41 cases). The incidence of the latter, compared to the previous epidemic, was higher (0.28 and 0.19% of the total population), including persons older than 15 years (0.19 and 0.12%). Thus, the influenza A(H1N1)pdm09 virus still remains the main cause of fatalities.
One of the reasons for the high incidence of influenza in the last epidemic may be the increase in influenza registration with increased PCR testing for influenza. The influence of interference between influenza and COVID-19 cannot be ruled out, with a decrease in COVID-19 incidence and an increase in influenza incidence in the last season.
1 Resolution of the Government of the Russian Federation of December 14, 2022 No. 2297 “On Amendments to Section IV of the Program of State Guarantees of Free Medical Assistance to Citizens for 2022 and for the Planning Period of 2023 and 2024” (publication number: 0001202212150010).
About the authors
Ludmila S. Karpova
Smorodintsev Research Institute of Influenza
Author for correspondence.
Email: epidlab@influenza.spb.ru
ORCID iD: 0000-0001-6621-5977
D. Sci. (Med.), Head, Laboratory of epidemiology of influenza and ARI
Russian Federation, St. PetersburgMaria Yu. Pelikh
Smorodintsev Research Institute of Influenza
Email: epidlab@influenza.spb.ru
ORCID iD: 0009-0003-1996-4512
researcher, Laboratory of epidemiology of influenza and ARI
Russian Federation, St. PetersburgKirill A. Stolyarov
Smorodintsev Research Institute of Influenza
Email: epidlab@influenza.spb.ru
ORCID iD: 0000-0002-1765-2799
leading programmer, Laboratory of epidemiology of influenza and ARI
Russian Federation, St. PetersburgKsenia M. Volik
Smorodintsev Research Institute of Influenza
Email: epidlab@influenza.spb.ru
ORCID iD: 0000-0002-5557-9318
leading programmer, Laboratory of epidemiology of influenza and ARI
Russian Federation, St. PetersburgTatyana P. Stolyarova
Smorodintsev Research Institute of Influenza
Email: epidlab@influenza.spb.ru
ORCID iD: 0009-0004-2882-0016
technician, Laboratory of epidemiology of influenza and ARI
Russian Federation, St. PetersburgDaria M. Danilenko
Smorodintsev Research Institute of Influenza
Email: epidlab@influenza.spb.ru
ORCID iD: 0000-0001-6174-0836
Cand. Sci. (Biol.), senior researcher, Deputy director for science
Russian Federation, St. PetersburgReferences
- Карпова Л.С., Столяров К.А., Пелих М.Ю. Совершенствование традиционной системы надзора в национальном центре по гриппу в условиях пандемии COVID-19 (2020–2023). Журнал инфектологии. 2024;16(2S1):245–6. Karpova L.S., Stolyarov K.A., Pelikh M.Yu. Improving the traditional surveillance system at the national influenza center during the COVID-19 pandemic (2020-23). Journal Infectology. 2024;16(2S1):245–6.
- Vega T., Lozano J.E., Meerhoff T., et al. Influenza surveillance in Europe: establishing epidemic thresholds by the moving epidemic method. Influenza Other Respir. Viruses. 2013;7(4):546–58. DOI: https://doi.org/10.1111/j.1750-2659.2012.00422.x
- Vega T., Lozano J.E., Meerhoff T., et al. Influenza surveillance in Europe: comparing intensity levels calculated using the moving epidemic method. Influenza Other Respir. Viruses. 2015;9(5):234–46. DOI: https://doi.org/10.1111/irv.12330
- Аношко О.Н., Лапо Т.П., Кищенко Е.Н., et al. Вклад вирусов гриппа, SARS-CoV-2 и других респираторных патогенов в этиологическую структуру возбудителей тяжелых острых респираторных инфекций в Республике Беларусь в 2021-2022 гг. В кн.: Сборник научных трудов «БГМУ – в авангарде медицинской науки и практики». Выпуск 12. Минск;2022:294–9. Anoshko O.N., Lapo T.P., Kisnchenko E.N., et al. Contribution of influenza viruses, SARS-CoV-2 and other respiratory pathogens to the etiological structure of severe acute respiratory infection causes in the Republic of Belarus in 2021–2022. In: Collection of Scientific Papers «BSMU – at the Forefront of Medical Science and Practice». Issue 12. Minsk;2022:294–9.
- Соминина А.А., Даниленко Д.М., Столяров К.А. и др. Интерференция SARS-CoV-2 с другими возбудителями респираторных вирусных инфекций в период пандемии. Эпидемиология и вакцинопрофилактика. 2021;20(4):28–39. Sominina A.A., Danilenko D.M., Stolyarov K.A., et al. Interference of SARS-CoV-2 with other respiratory viral infections agents during pandemic. Epidemiology and Vaccinal Prevention. 2021;20(4):28–39. DOI: https://doi.org/10.31631/2073-3046-2021-20-4-28-39 EDN: https://elibrary.ru/cdrnsj
- Горенчук А.Н., Жоголев С.Д., Жоголев К.Д. и др. Изменение этиологии острых болезней органов дыхания в организованных коллективах в период пандемии COVID-19 по сравнению с доковидным периодом. В кн.: Микробиология военной медицине и здравоохранению. Современные технологии: наука, практика, инновации: Материалы Всероссийской научно-практической конференции, посвященной 100-летию со дня основания кафедры микробиологии Военно-медицинской академии имени С.М. Кирова. СПб.;2023:28–34. Gorenchuk A.N., Zhogolev S.D., Zhogolev K.D., et al. Changes in the etiology of acute respiratory diseases in organized groups during the COVID-19 pandemic compared to the pre-COVID period. In: Microbiology to Military Medicine and Healthcare. Modern Technologies: Science, Practice, Innovation: Materials of the All-Russian Scientific and Practical Conference Dedicated to the 100th Anniversary of the Founding of the Department of Microbiology of the Military Medical Academy named after S.M. Kirov. St. Petersburg;2023:28–34.
- Аношко О.Н., Лапо Т.П., Кищенко Е.Н. и др. Эпидемический процесс по гриппу во время пандемии COVID-19 в Республике Беларусь. В кн.: Вирусные инфекции – от диагностики к клинике: сборник тезисов Всероссийской конференции молодых ученых. СПб.;2023:10–1. Anoshko O.N., Lapo T.P., Kishchenko E.N., et al. Epidemic process of influenza during the COVID-19 pandemic in the Republic of Belarus. In: Viral Infections — from Diagnosis to Clinic: Collection of Abstracts of the Russian Conference of Young Scientists. St. Petersburg;2023:10–1.
- Дорош А.В., Смородинцева Е.А., Столяров К.А. Этиология ТОРИ в период пандемии COVID-19 по данным сигнального надзора. В кн.: Вирусные инфекции – от диагностики к клинике: сборник тезисов Всероссийской конференции молодых ученых. СПб.;2024:16–7. Dorosh A.V., Smorodintseva E.A., Stolyarov K.A. Etiology of SARI during the COVID-19 pandemic according to sentinel surveillance data. In: Viral Infections – from Diagnosis to Clinic: Collection of Abstracts of the Russian Conference of Young Scientists. St. Petersburg;2024:16–7.
- Переяслов Д.И., Ибадуллаева Н.С., Рахимов Р.А. и др. Эпидемическая обстановка по гриппу и ОРВИ в сезон 2023–2024 гг. Журнал инфектологии. 2024;16(2S1):275. Pereyaslov D.I., Ibadullayeva N.S., Rakhimov R.A., et al. The epidemic situation of influenza and ARI in the 2023-2024 season. Journal Infectology. 2024;16(2S1):275.
- Аншелес И.М., Фридман Э.А., Стенина Е.С. и др. Некоторые итоги эпидемиологических, иммунологических и вирусологических сопоставлений по материалам эпидемических волн гриппа типа А2 1957 и 1959гг. в Ленинграде. В кн.: Этиология, иммунология и клиника азиатского гриппа: Труды института экспериментальной медицины АМН СССР. Л.;1961:138–47. Ansheles I.M., Fridman E.A., Stenina E.S., et al. Some results of epidemiological, immunological and virological comparisons based on materials from the epidemic waves of influenza type A2 in 1957 and 1959 in Leningrad. In: Etiology, Immunology and Clinic of Asian Influenza: Proceedings of the Institute of Experimental Medicine of the USSR Academy of Medical Sciences. Leningrad;1961:138–47.
- Смородинцев А.А. Итоги изучения этиологии и иммунологии азиатского гриппа типа А2 в Ленинграде. В кн.: Этиология, иммунология и клиника азиатского гриппа: Труды института экспериментальной медицины АМН СССР. Л.;1961:127–37. Smorodintsev A.A. Results of the study of the etiology and immunology of Asian influenza type A2 in Leningrad. In: Etiology, Immunology and Clinic of Asian Influenza: Proceedings of the Institute of Experimental Medicine of the USSR Academy of Medical Sciences. Leningrad;1961:127–37.
- Карпухин Г.И. Особенности распространения гриппа А1 в мире и СССР. В кн.: Проблемы гриппа и острых респираторных заболеваний: Сборник научных трудов ВНИИ гриппа. Том 2. Л.;1979:5–17. Karpukhin G.I. Features of the spread of influenza A1 in the world and the USSR. In: Problems of Influenza and Acute Respiratory Diseases: Collection of Scientific Works of Russian Research Institute of Influenza. Volume 2. Leningrad;1979:5–17.
- Карпова Л.С., Маринич И.Г., Поповцева Н.М., Столярова Т.П. Эпидемиология гриппа А(H1N1) Калифорния/07/09 среди населения 49 городов России в сезон 2009–2010 гг. Журнал микробиологии, эпидемиологии и иммунобиологии. 2011;88(3):14–20. Karpova L.S., Marinich I.G., Popovtseva N.M., Stolyarova T.P. Epidemiology of influenza A/CALIFORNIA/07/09 (H1N1) in population of 49 cities in Russia in 2009–2010. Journal of Microbiology, Epidemiology and Immunobiology. 2011;88(3):14–20. EDN: https://elibrary.ru/rsypel
- Карпова Л.С., Бурцева Е.И., Поповцева Н.М., Столярова Т.П. Сравнение эпидемий гриппа в России 2009 и 2011 годов, вызванных пандемическим вирусом гриппа А(H1N1). Эпидемиология и вакцинопрофилактика. 2012;60(5):6–15. Karpova L.S., Burtseva E.I., Popovtseva N.M., Stolyarova T.P. Comparison of influenza epidemics in Russia 2009 and 2011, caused by pandemic influenza A(H1N1). Epidemiology and Vaccinal Prevention. 2012;60(5):6–15. EDN: https://elibrary.ru/oiiecn
Supplementary files