Human blood granulocyte degranulation and lysis intensity during interaction with Yersinia pestis in the ex vivo model of bacteriemia
- Authors: Kravtsov A.L.1, Bugorkova S.A.1, Klyueva S.N.1, Shmelkova T.P.1, Kozhevnikov V.A.1
-
Affiliations:
- Russian Anti-Plague Institute "Microbe"
- Issue: Vol 102, No 1 (2025)
- Pages: 80-90
- Section: ORIGINAL RESEARCHES
- URL: https://microbiol.crie.ru/jour/article/view/18500
- DOI: https://doi.org/10.36233/0372-9311-481
- EDN: https://elibrary.ru/OPXPGY
- ID: 18500
Cite item
Abstract
Introduction. Considering the decisive role of antibacterial strategies of secretory degranulation and NETosis in the prevention of sepsis, it is of interest to study the interaction of Yersinia pestis with human blood granulocytes using an ex vivo bacteremia model to assess the effectiveness of this antibacterial strategy of the host organism in plague.
Purpose: evaluation of granulocyte degranulation and lysis in human whole blood samples in the presence of live Y. pestis.
Materials and methods. Bacteremia was modeled by adding Y. pestis EV NIIEG cells grown at 37оC or 28оC to whole blood (with heparin) at a dose of 108 mc/mL. Strains Staphylococcus aureus ATCC 6538 (209-P) and Escherichia coli ATCC 25922 were used in experiments with blood from the same donors as a positive control. The bactericidal effect was determined at different time points during blood incubation at 37оC (for 6 hours) using a microbiological method. Using flow cytometry, immunophenotyping of leukocytes was performed in the blood according to the Lyse/No-Wash protocol to determine the expression of the main leukocyte antigen CD45 and the secretory azurophilic degranulation marker CD63 on the surface of the granulocytes. The intensity of granulocyte lysis was assessed by the decrease in the proportion of these cells in the total leukocyte population.
Results. It has been established that live plague microbes, unlike E. coli and S. aureus, do not cause the development of azurophilic degranulation in human blood granulocytes and do not induce autolysis (NETosis) of these cells within 6 hours when bacteremia is modeled ex vivo.
Conclusion. Information was obtained on the ability of the plague microbe to suppress the extracellular bactericidal mechanisms of granulocytes in the blood of people not vaccinated against plague, which effectively function under conditions of bacteremia against E. coli and S. aureus. An experimental and methodological basis has been prepared for further research with blood cells from donors vaccinated against plague in order to develop new effective tests for assessing the intensity of acquired cellular anti-plague immunity in humans.
Full Text
Introduction
Primary pneumonic plague, caused by Yersinia pestis and transmitted to humans through respiratory droplets from another person or domestic animal, is the most dangerous bacterial infection, in which the pathogen effectively neutralizes the protective mechanisms of the immune system and multiplies intensively in the host organism without inducing the development of an in vivo protective inflammatory response for a long time. The asymptomatic character of the development of the infectious process during the first 2 days after aerogenic infection with plague is the key factor determining the high epidemic danger of primary pneumonic plague [1, 2]. The pathogenesis of plague is poorly understood, especially at the stage of bacteremia [3], when Y. pestis cells resistant to phagocytosis, proliferating extracellularly in microcapillaries of the liver, lungs and other organs, enter in vivo into prolonged contact interaction with peripheral blood leukocytes, including neutrophil granulocytes (NG), responsible for the development of inflammatory reactions [4].
Nevertheless, in experiments on laboratory animals, an important feature of the pathogenetic mechanism of primary pneumonic plague has been established, which consists of the complete suppression of the inflammatory processes at the early stage of infection, such as secretory azurophilic degranulation [5], chemotaxis [6], apoptosis [7] and lysis of NG [8] by effector Yop-proteins (Yersinia outer proteins) synthesized by Y. pestis at 37°C and secreted by extracellularly multiplying plague microbes into the cytoplasm of cells of the host immune system [4, 9]. At the same time, Yop virulence proteins of Y. pestis, on the contrary, trigger the death of macrophages by apoptosis, which disrupts the in vivo functioning of the efferocytosis mechanism and inevitably leads to the generalization of the inflammatory process as a result of massive autolysis of peripheral blood NG unable to realize their bactericidal potential. Autolysis of granulocytes, rapidly triggered with a time delay in the whole organism at once, according to the hypothesis of M.T. Silva [10], leads to the release of a huge amount of leukocyte elastase (LE) molecules into the blood plasma, destroying elastin of the lungs and blood vessels, as well as cleaving cell receptors and plasma proteins responsible for the regulation of the coagulation process, which is the trigger for the unexpected and lightning fast development of sepsis in primary pneumonic plague.
To confirm (or refute) this hypothesis, a detailed study of the processes of degranulation and lysis of human and animal blood granulocytes using modern methods of cytological analysis under conditions of ex vivo modeling of plague bacteremia is required. As evidenced by the results of the study of COVID-19 pathogenesis associated with a pronounced imbalance in the elastase-inhibitor system [11], in the case of isolation of NG from the peripheral blood of patients, important information about the role of NETosis in immunological defense and in the development of the process of hypercoagulation in sepsis may be lost, because the procedure of centrifugation of blood cells in a density gradient does not allow differentiating from lymphocytes and monocytes the population of activated low-density NG prone to NETosis with increased expression of the marker of azurophilic degranulation CD63 on the cell surface [12].
For a long time, studies on ex vivo models of bacteremia were not performed, including in experiments with opportunistic bacteria [13], because it was believed that blood granulocytes realize their powerful bactericidal potential only after migration from the vascular channel to tissues, where they neutralize bacteria by phagocytosis. The situation changed after the discovery of NETosis in 2004 and the studies of V. McDonald et al. [14], who experimentally proved that autolysis of NG (NETosis), preceded and accompanied by secretory azurophilic degranulation of NG with release from LE granules, allows the organism to neutralize microbes at an early stage of bacteremia (during the first 6 h) directly in the blood stream with the help of NET (Neutrophil Extracellular Traps) DNA networks, launched by activated neutrophils into the extracellular space. Moreover, the efficiency of this previously unknown mechanism of immunological defense in terms of preventing bacterial sepsis in infections caused by Escherichia coli and Staphylococcus aureus was 4 times higher than phagocytosis.
In particularly dangerous infections, the pathogens of which are resistant to digestion in macrophages (e.g., Y. pseudotuberculosis), proteases and bactericidal cationic proteins released from NG during secretory degranulation and cytolysis partially or completely neutralize phagocytosis-resistant bacteria, which after such pre-treatment are rapidly absorbed and digested by macrophages [15]. In 2002, for the first time, we published the results of studies in which the flow cytofluorimetric method of assessing the intensity of degranulation was used to record differences in the ability of plague microbes grown at 28°C and 37°C to trigger ex vivo the process of secretory degranulation in human whole blood phagocytes. Cells grown at 37°C were characterized by a breakdown of antibacterial response by the indicator of secretory degranulation in the model of plague bacteremia [16]. Many years later, experimental data began to appear in the foreign press, which could explain the mechanism of the phenomenon of the absence of phagocyte degranulation in human blood contaminated with live plague microbes. The studies were carried out in vivo in mice [5, 8] and in vitro with NG previously isolated from human blood [17, 18]. Degranulation was assessed, in contrast to our work, not using supravital staining with acridine orange (AO) dye, but by the degranulation marker CD63. Experiments in an ex vivo model of bacteremia were not performed. The intensity of granulocyte lysis in human blood contaminated with plague microbes or opportunistic microorganisms had not been determined or controlled by flow cytometry before our study was conducted.
The relevance of continuing our earlier studies on the ex vivo model of bacteremia using the marker of azurophilic degranulation CD63 and other leukocyte phenotypic markers was determined by the need to develop a cellular test for assessing the intensity of post-vaccination plague immunity in humans, based on quantitative assessment of the damage of peripheral blood neutrophils by specific antigen. In light of modern ideas, the strategy of vaccine development for emergency prophylaxis of plague and other particularly dangerous infections should take into account the ability of immunostimulating drugs to trigger the mechanism of extracellular antibody-dependent cytotoxicity (bactericidality) of NG [19], realized in the blood by interaction with antigen-antibody immune complexes through the processes of secretory azurophilic degranulation and NETosis [20]. Only when specific antibodies to the antigen previously used for immunization of animals appear in the blood, intravenous injection (or addition to the blood) of this antigen triggers in the body (or under ex vivo conditions) a protective IgG-mediated anaphylactic reaction associated with secretory degranulation and lysis of peripheral blood NGs [21]. The molecular mechanisms responsible for the transition of the infectious process in primary pneumonic plague from the asymptomatic to the systemic inflammation phase are poorly understood [3, 22], and one of them may be related to the in vivo triggering of an IgG-mediated allergic reaction.
The absence of a local protective inflammatory response in a non-immune host organism is observed not only when infected with wild virulent strains of Y. pestis, but also in response to non-pigmented strains with a virulence plasmid, such as the vaccine strain of Y. pestis, but also in response to non-pigmented strains with a virulence plasmid, which includes the vaccine strain of Y. pestis EV NIIEG (Pgm¬-pFra+pCad+pPst+) [1, 23]. Possessing residual virulence, such attenuated strains cause death of laboratory animals only when administered intravenously in doses of more than 106 mc, which is used in model experiments to study the mechanisms of immunity and virulence [23].
The aim of the present study was to evaluate degranulation and lysis of granulocytes in human whole blood samples in the presence of live Y. pestis.
Materials and methods
The attenuated Y. pestis EV NIIEG strain was used in the studies, S. aureus strain ATSS 6538 (209-P) and E. coli strain ATSS 25922 from the State Collection of Pathogenic Bacteria of the Russian Anti-Plague Institute Microbe of Rospotrebnadzor. Daily cultures of S. aureus and E. coli were grown on Hottinger’s agar (pH 7.2) at 37°C. For Y. pestis EV cells, a two-day stationary bacterial culture grown on the same agar at 28°C (Y.pestis28) was obtained. An exponential 18-h culture of Y. pestis EV with altered antigenic properties was obtained by growing on Hottinger broth (pH 7.2) with aeration at 37°C (Y.pestis37) [24]. In sterile phosphate-salt buffer (pH 7.4) with 0.9% NaCl, suspensions of live bacteria with a concentration of 109 mc/ml from cultures of E. coli, S. aureus, Y.pestis28 and Y.pestis37 were prepared according to the standard turbidity sample CCA 42-28-59-85P.
The study involved 10 conditionally healthy unvaccinated against plague donors (3 men and 7 women) aged 25–55 years who gave written voluntary informed consent to participate in the study. The study protocol was approved by the Ethical Committee of the Russian Research Anti-Plague Institute Microbe (Protocol No. 9 of 21.10.2020).
Blood from volunteers was drawn into tubes with anticoagulant (heparin) and used for 1–2 h. To simulate bacteremia, 100 μL of the tested billionth bacterial suspension was added to 1 ml of blood containing on average 2 × 106 phagocytes, which corresponded to a concentration of 108 mc/mL of blood or an initial microbial load (number of bacteria : phagocyte) of 50 : 1 on average [25]. With blood from each donor, cell suspensions of Y. pestis28 and Y.pestis37 were examined simultaneously with cell suspensions of E. coli and/or S. aureus. Blood samples (1 mL each) with the tested bacteria were placed in the shaker-incubator ES-20 (BioSan) and incubated under stirring for 6 hours. Samples incubated for 6 h without bacteria with 100 μL of sterile phosphate-salt buffer per 1 mL of blood served as a control.
Immunophenotyping of leukocytes in the studied blood samples for flow cytofluorimetric analysis was performed according to the Lyse/No-Wash protocol [26] using labeled mouse monoclonal antibodies to human leukocyte antigens CD45-FITC and CD63-PE (Bekman Coulter). Granulocytes were identified by the degree of their intracellular granularity (side light scattering intensity) and by the expression of total leukocyte antigen (CD45). The relative content of cells positive for the expression of the azurophilic degranulation surface marker CD63 was determined in the granulocyte gate [5, 17]. The results were taken into account for each experimental and control blood sample in dynamics: after 0, 1, 2, 4, 6 h of incubation.
The total number of live bacteria in blood (in plasma and within active phagocytes) was determined by a microbiological method based on osmotic lysis of blood cells in distilled water [27]. To 1 mL of H2O, 10 µL of blood was added. After 30 s, serial 10-fold dilutions of plasma containing bacteria and blood cell lysis products were prepared in phosphate-salt buffer from water-diluted plasma containing bacteria and blood cell lysis products for seeding on dishes with Hottinger’s agar (pH 7.2). For each dilution, the number of colony forming units (CFU) of Staphylococcus aureus or Escherichia coli were counted after one day of growth at 37°C, and Y. pestis cells were counted on the 3rd day of growth at 28°C. In relation to the number of CFU after 0 h of incubation, taken as 100%, the survival rate of bacteria of each species in blood (in %) after 1, 2 and 6 h of incubation was estimated to comparatively characterize the development of bactericidal effect under ex vivo conditions [25].
The intensity of granulocyte lysis was quantified ex vivo by flow cytometry by a decrease in the proportion of these cells in whole peripheral blood samples, as well as by an increase in the relative content of cellular debris in the blood [25].
To assess the light scattering and immunofluorescence intensity of CD-marker-labeled blood leukocytes, a DakoCytomation (Dako) flow cytometer with Summit v.4.3 Built 2445 software was used.
The obtained experimental data were statistically processed using the standard Microsoft Office Excel 2016 software package, Statistica 10.0 (StatSoft Inc.), presenting the results in the form of median (Me) and quartile deviations [Q1; Q3] with calculation of the reliability of differences in the studied groups using the Mann–Whitney U-criterion. A value of p < 0.05 was considered significant.
Results
When Y.pestis37 was added to blood for 6 h, granulocytes lacked changes related to the state of cytoplasmic granules, as well as lysis of these cells under conditions of ex vivo modeling of plague bacteremia, while in the blood of the same donors opportunistic bacteria induced intensive degranulation and inevitable lysis of the overwhelming majority of granulocytes in the total population of peripheral blood leukocytes by 6 h of incubation. Antibacterial response of granulocytes according to the studied indicators of degranulation and cytolysis took place in the case of ex vivo modeling of bacteremia by Y.pestis28 cells. However, in comparison with the reaction to E. coli or S. aureus, this response was significantly less intense (Table).
The results of granulocyte azurophilic degranulation and lysis intensity estimation in an ex vivo modeling of bacteremia by live E. coli, S. aureus and Y.pestis37 in depending of blood incubation time at 37oC, Me [Q1; Q3]
Parameter | Blood sample | Duration of incubation, min | |||
60 | 120 | 240 | 360 | ||
Granulocyte lysis intensity, % | Сontrol | 5,2 | 9,1 | 12,2 | 14,6 |
S. aureus | 27 | 56,0 | 78 | 82,0 | |
E. coli | 22,3 | 38,8 | 63,6 | 78,6 | |
Y.pestis28 | 7,3 | 10,4 | 20,6 | 19,0 | |
Y.pestis37 | 6,7 | 8,0 | 9,3 | 10,6 | |
Share of granulocytes with CD63+ phenotype, % | Сontrol | 10 | 14 | 17 | 18 |
S. aureus | 35 | 70 | 83 | 79 | |
E. coli | 28,3 | 50,3 | 70,6 | ||
Y.pestis28 | 19,7 | 26,0 | 32,3 | 31,2 | |
Y.pestis37 | 14,2 | 13,4 | 15,1 | 20,8 | |
Note. *p < 0.05 compared with control.
The registered differences in the studied parameters are clearly illustrated by the example of Y.pestis37 and E. coli characteristic cytograms presented in Fig. 1, where granulocytes are localized by the degree of intracellular granularity (intensity of lateral light scattering) and density of CD45 expression in the ellipse-shaped region R3 at their automatic differentiation from lymphocytes and monocytes in control blood samples. In the presence of E. coli, the proportion of granulocytes (cells in the R3 region) decreased after 6 h in the total leukocytic population relative to the control index by 10 times – from 47.1% to 4.8%, and in the presence of Y.pestis37 actually did not change, remaining close to the control (43.8%). In blood contaminated with E. coli, the proportion of granulocytes decreased sharply during this period due to massive lysis of dead phagocytes, significantly increasing the relative amount of signals from cellular debris registered outside the R1 region. On the cytogram of the experimental blood sample with Y.pestis37 cells, the proportion of debris after 6 h of incubation was, on the contrary, lower than in the control without bacteria.
Fig. 1. Cytograms of the blood leukocyte distribution according to the degree of intracellular granularity and the cell surface common leukocyte antigen CD45 expression density at 6 h after the addition of Y. pestis and E. coli to the blood of the same donor.
Regions R3 and R2 correspond to granulocytes and lymphocytes. Monocytes are localized in the area between the R2 and R3 regions. All intact undamaged leukocytes were counted by the cytometer in the R1 region, beyond which signals from cellular debris, products of the breakdown of leukocytes with a low level of leukocyte antigen expression, accumulated. The proportion of cells in each region is expressed as a percentage of the total number of registered leukocytes. The proportion of debris corresponds to (100 – R1)%.
In contrast to opportunistic bacteria, Y.pestis37 cells did not induce ex vivo increased expression on the granulocyte surface of the lysosomal protein CD63 (tetraspanin), which is a marker of the development of secretory azurophilic degranulation (Fig. 2). In blood samples contaminated with live E. coli and S. aureus cells, the process of CD63 secretion from granules to the granulocyte surface began after one hour, significantly intensified from the 2nd hour of incubation and preceded the lysis of activated granulocytes under ex vivo conditions (Table).
Fig. 2. Relative content of activated cells with CD63+ phenotype in the granulocyte gate after 2 h of ex vivo interaction with living cells of Y.pestis37, E. coli and S. aureus.
CD63+ granulocytes are localized in the R1 region of cytograms; control is the blood after 2 h without bacteria. The proportion of cells in R1 region is expressed as a percentage of the total number of registered granulocytes.
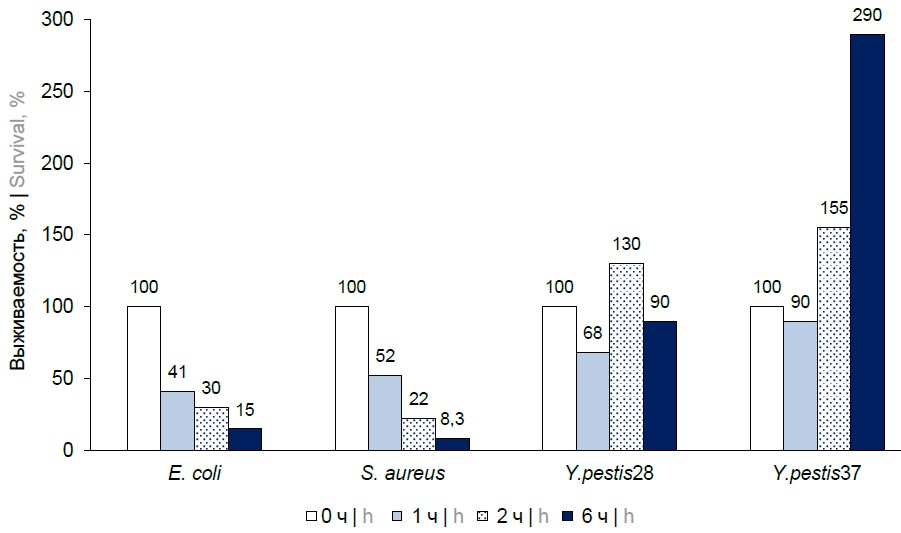
Against the background of the absence of antibacterial response of granulocytes according to the studied indicators of degranulation and leukocytolysis, increased survival of Y.pestis37 in human whole blood samples in comparison with Y.pestis28 was registered by the microbiological method. The plague microbe grown at the temperature of the host organism began to multiply intensively after 6 h under conditions of ex vivo modeling of bacteremia. In the blood of the same donors, opportunistic bacteria were quickly killed under the influence of bactericidal effect of active phagocytes. The survival rate of E. coli and S. aureus decreased by at least 80% by 6 h from the moment of bacteremia modeling (Fig. 3).
Fig. 3. Increased survival of Y.pestis37 in human blood compared to E. coli, S. aureus and Y.pestis28 in an ex vivo bacteremia model.
Discussion
When conducting the present study by flow cytometry, experimental data were obtained for the first time indicating that the Lyse/No Wash procedure for immunophenotyping of blood leukocytes using fluorochrome-labeled CD markers, which excludes cell losses and the effect of centrifugation on cells [26], allows rapid assessment in human whole blood samples of both the intensity of the secretory degranulation process and granulocyte autolysis triggered by an infectious agent ex vivo at the initial stage of bacterial modeling. Because of experiments with E. coli and S. aureus, new information has been obtained that confirms the importance of rapid development of degranulation and granulocyte autolysis processes in blood for the killing of these bacteria under conditions of bacteremia, as previously established in animal experiments [14], using human cell models. The inability of Y.pestis37 cells multiplying intensively in the blood to trigger functional activation of granulocytes by secretory degranulation and cytolysis is important for understanding the causes of asymptomatic development of the infectious process in primary pneumonic plague [10, 22]. The results of microbiological studies obtained simultaneously with the data of cytofluorimetric analysis in an ex vivo model may help to explain why plague bacteremia always inevitably leads to sepsis unlike staphylococcal bacteremia.
Y.pestis37 cells proliferating in human blood at 37°C did not trigger the secretion of lysosomal protein tetraspanin (CD63) from the primary granules of granulocytes to the cell surface, which is consistent with the results of studies by K.R. Eichelberger et al. conducted in vivo on laboratory animals [5] and in vitro on the model of NG previously isolated from human blood [17]. In this regard, the fact that CD63 protein is involved in the process of secretion from the same granules of LE [28], which is a generally recognized biochemical marker of the inflammatory process [29] and a key protein of innate antibacterial defense, responsible for rapid selective cleavage of virulence factors of Yersinia spp. and other Enterobacteriaceae in the focus of infectious inflammation, may be of great importance [30].
To kill bacteria in blood plasma and other biological fluids, this protease forms antibacterial peptides with broad-spectrum antibiotic properties from inactive lysosomal precursor proteins during degranulation [31]. By cleaving histones in the nuclei of activated neutrophils, LE triggers and regulates, together with myeloperoxidase, the process of decondensation of nuclear chromatin during NETosis, in which the autolysis of NG is accompanied by the release into the blood and tissues of the body of DNA nets with the products of NG decay adsorbed in them, which have pronounced bactericidal properties (LE and myeloperoxidase, histones, antibacterial peptides, etc.). [32].
The information presented in the table about the intensity of azurophilic degranulation ex vivo by CD63 marker is confirmed by the results of our earlier studies, in which phagocyte degranulation was assessed by supravital staining of cells with AO dye [16] and the viability of granulocytes in blood with Y. pestis and S. aureus cells was monitored by flow cytometry by identifying and counting the number of dead diploid cells with reduced (less than 2C) DNA content [24, 33]. It is known that blood granulocytes accumulate AO dye in much larger amounts than lymphocytes and monocytes in the form of its positively charged form AOH+, which is formed and accumulated in the granules of living cells in the process of continuous pumping of H+ protons through intact membranes of lysosomes [34]. The level of AO accumulation in azurophilic granules depends on the amount of LE molecules in them, and in the process of degranulation, LE is released from the granules into the extracellular space together with AO molecules [35]. In blood contaminated with live S. aureus cells, granulocytes lost the initially intense red fluorescence of their granules between 3 and 4 h of incubation. The preservation of intense fluorescence of granulocytes in the analysis of blood samples contaminated with live cells of Y.pestis37 indicated the absence of degranulation in phagocytes at the early stage of ex vivo modeling of plague bacteremia, the stability of azurophilic granule membranes in peripheral blood granulocytes retaining their viability during 6 h of incubation [16].
In a study by S.C. Dudte et al., in which the degranulation of human NG isolated from blood was evaluated in vitro in interaction with Y. pestis and S. aureus both by CD63 expression and LE expression on the cell surface, only live Staphylococcus aureus induced in vitro intensive degranulation [18]. Our data obtained in experiments with attenuated strain of Y. pestis EV NIIEG on the ex vivo model of bacteremia agree with the conclusions of S.C. Dudte et al. However, the model we used was more informative because it allowed us to additionally assess the intensity of leukocytolysis in blood by flow cytometry.
The lower content of cellular debris registered by us in blood with cells of Y. pestis cells after 6 h of incubation, compared to control blood samples without bacteria, can be explained by the ability of Y.pestis37 to suppress spontaneous apoptosis and lysis of granulocytic cells at the early stage of infection, as known from animal experiments [7, 8, 10].
The reason for the intensive multiplication and rapid spread of Y. pestis in the host organism is explained by a change in the structure of its lipopolysaccharide (LPS) when the temperature rises from 28°C to 37°C. It is believed that Y. pestis does not induce a protective inflammatory response in the organism at LPS due to the inability of its structurally altered LPS to stimulate TLR4 cells of innate immunity [36]. This explanation does not contradict the results of our studies, since LPS of Gram-negative bacteria is a powerful inducer of secretory degranulation of NG with the release of CD63 and LE on the cell surface and in the extracellular space [37]. However, the proteolytic effect of LE released from phagocyte granules, which determines the ability of this receptor to respond to the presence of LPS in vivo, was found to be necessary for TLR4 activation [22]. It is known that tolerance to high doses of endotoxin is formed in mice when the organism is exposed to LPS for a long time (with repeated intravenous administration of low doses over several days). Neutrophils of tolerant animals more effectively neutralized pathogenic bacteria due to the in vivo inclusion of an additional mechanism of antibacterial defense (NETosis), which did not function in the organism of intact animals [38]. According to our data, a live plague vaccine had a similar effect on mice, forming intense post-vaccination anti-plague immunity in animals of this species [39].
In the present study, we do not present experimental data on the identification and determination of NG content in blood by their specific phenotypic marker CD16 (FcᵧRIIIb receptor) in order not to complicate its description. Since the proportion of NG in the total population of blood granulocytes in the samples studied by us was more than 90% [25] and corresponded to clinically established normal values of this index [12], the possibility to call the total population of granulocytes NG when discussing the obtained experimental data is allowed in our study.
The flow cytometry method is known to differentiate IgG-dependent anaphylaxis associated with activation of the secretory function of peripheral blood neutrophils from IgE-dependent anaphylactic reaction that develops as a result of stimulation of mast cells and basophils [40]. It is possible that when functionally active IgG-antibodies to specific antigens of Y. pestis appear in the blood, they will activate the mechanism of extracellular antibody-dependent cytotoxicity of NG, which can be registered by flow cytometry on the ex vivo model according to the intensity of degranulation and lysis of peripheral blood granulocytes. Such analysis may be more sensitive and informative than in cases when an alternative skin test indicator of neutrophil damage is subjectively assessed in practice in human whole blood samples using a long and laborious method of microscopic analysis.
Conclusion
The study of degranulation processes and lysis of granulocytes in human whole blood samples infected with live Y. pestis, helped obtain new information using CD markers and flow cytometry, indicating that the mechanisms of extracellular granulocyte bactericidal activity, which function effectively against E. coli and S. aureus, do not work at the early stage of bacteremia in the blood of people unvaccinated against plague. In ex vivo modeling of bacteremia using the attenuated strain of Y. pestis EV NIIEG has created the necessary experimental and methodological basis for further study of the processes of degranulation and lysis of NG in blood samples of people inoculated against plague, for the development of new, more effective tests to assess the intensity of acquired cellular anti-plague immunity.
About the authors
Aleksandr L. Kravtsov
Russian Anti-Plague Institute "Microbe"
Author for correspondence.
Email: kravzov195723@gmail.com
ORCID iD: 0000-0002-9016-6578
D. Sci. (Biol.), leading researcher, Department of immunology
Russian Federation, SaratovSvetlana A. Bugorkova
Russian Anti-Plague Institute "Microbe"
Email: rusrapi@microbe.ru
ORCID iD: 0000-0001-7548-4845
D. Sci. (Med.), chief researcher, Department of immunology
Russian Federation, SaratovSvetlana N. Klyueva
Russian Anti-Plague Institute "Microbe"
Email: klyueva.cvetlana@mail.ru
ORCID iD: 0000-0002-5550-6063
Cand. Sci. (Biol.), researcher, Department of immunology
Russian Federation, SaratovTatyana P. Shmelkova
Russian Anti-Plague Institute "Microbe"
Email: training@microbe.ru
ORCID iD: 0000-0001-5891-6028
Cand. Sci. (Biol.), senior researcher, Department of educational programs and specialist training
Russian Federation, SaratovVitaly A. Kozhevnikov
Russian Anti-Plague Institute "Microbe"
Email: 787868@mail.ru
ORCID iD: 0000-0001-7267-7027
junior researcher, Department of immunology
Russian Federation, SaratovReferences
- Домарадский И.В. Очерки патогенеза чумы. М.;1966. Domaradskiy I.V. Essays on the Pathogenesis of Plague. Moscow;1966.
- Lathem W.W., Crosby S.D., Miller V.L., Goldman W.E. Progression of primary pneumonic plague: a mouse model of infection, pathology, and bacterial transcriptional activity. Proc. Natl. Acad. Sci. USA. 2005;102(49):17786–91. DOI: https://doi.org/10.1073/pnas.0506840102
- Подладчикова О.Н. Современные представления о молекулярных механизмах патогенеза чумы. Проблемы особо опасных инфекций. 2017;(3):33–40. Podladchikova O.N. Modern views on molecular mechanisms of plague pathogenesis. Problems of Particularly Dangerous Infections. 2017;(3):33–40. DOI: https://doi.org./10.21055/0370-1069-2017-3-33-40 EDN: https://elibrary.ru/zhgvxr
- Silva M.T., Silva Pestana N.T. The in vivo extracellular life of intracellular parasites: role in pathogenesis. Immunobiology. 2013;18(3):325–37. DOI: https://doi.org/10.1016/j.imbio.2012.05.011
- Eichelberger K.R., Jones G.S., Goldman W.E. Inhibition of neutrophil primary granule release during Yersinia pestis pulmonary infection. mBio. 2019;10(6):e02759-19. DOI: https://doi.org/10.1128/mBio.02759-19
- Eisele N., Lee-Lewis H., Besch-Williford C., et al. Chemokine receptor CXCR2 mediates bacterial clearance rather than neutrophil recruitment in a murine model of pneumonic plague. Am. J. Pathol. 2011;178(3):1190–200. DOI: https://doi.org/10.1016/j.ajpath.2010.11.067
- Spinner J.L., Seo K.S., O'Loughlin J.L., et al. Neutrophils are resistant to Yersinia YopJ/P-induced apoptosis and are protected from ROS-mediated cell death by the Type III secretion system. PLoS One. 2010;5(2):e9279. DOI: https://doi.org/10.1371/journal.pone.0009279
- Stasulli N.M., Eichelberger K.R., Price P.A., et al. Spatially distinct neutrophil responses within the inflammatory lesions of pneumonic plague. mBio. 2015;6(5):e01530-15. DOI: https://doi.org/10.1128/mBio.01530-15
- Spinner J.L., Cundiff J.A., Kobayashi S.D. Yersinia pestis type III secretion system-dependent inhibition of human polymorphonuclear leukocyte function. Infect. Immun. 2008;76(8):3754–60. DOI: https://doi.org/10.1128/IAI. 000385-08
- Silva M.T. Bacteria-induced phagocyte secondary necrosis as a pathogenicity mechanism. J. Leukoc. Biology. 2010;88(5):885–96. DOI: https://doi.org/10.1189/jlb.0410205
- Zerimech F., Jourdain M., Ouraed B., et al. Protease-antiprotease imbalance in patients with severe COVID-19. Clin. Chem. Lab. Med. 2021;59(8):e330–4. DOI: https://doi.org/10.1515/cclm-2021-0137
- Morrissay S., Geller A.E., Hu X., et al. A specific low-density neutrophil population correlates with hypercoagulation and disease severity in hospitalized COVID-19 patients. JCI Insight. 2021;6(9):e148435. DOI: https://doi.org/10.1172/jci.insight.148435
- Zwack E.E., Chen Z., Delvin J.C., et al. Staphylococcus aureus induces a muted host response in human blood that blunts the recruitment of neutrophils. Proc. Natl. Acad. Sci. USA. 2022;119(31): e2123017119. DOI: https://doi.org/10.1073/pnas.2123017119
- МсDonald B., Urrutia R., Yipp B.G., et al. Intravascular neutrophil extracellular traps capture bacteria from bloodstream during sepsis. Cell Host Microbe. 2012;12(3):324–33. DOI: https://doi.org/10.1016/j.chom.2012.06.011
- Исачкова Л.М., Плехова Н.Г. К развитию представлений об антиинфекционной резистентности. Эпидемиология и инфекционные болезни. 2002;(1):11–5. Isachkova L.M., Plekhova N.G. To the development of ideas about anti-infective resistance. Epidemiology and Infectious Diseases. 2002;(1):11–5.
- Kravtsov A.L., Bolyleva E.V., Grabenyukova T.P., et al. Flow microfluorometric analysis of phagocyte degranulation in bacteria infected whole blood cell cultures. In: Proceedings of Saratov Fall Meeting 2001: Optical Technologies in Biophysics and Medicine. Volume 4707. Saratov;2002:395–402. DOI: https://doi.org/10.1117/12.475607
- Eichelberger K.R., Goldman W.E. Human neutrophil isolation and degranulation responses to Yersinia pestis infection. In: Vadyvaloo V., Lawreuz M., eds. Pathogenic Yersinia. Methods in Molecular Biology. New York;2019:197–209. DOI: https://doi.org/10.1007/978-1-4939-9541-7
- Dudte S.C., Hinnebusch B.J., Shannon J.G. Characterization of Yersinia pestis interactions with human neutrophils in vitro. Front. Cell. Infect. Microbiology. 2017;7:358–65. DOI: https://doi.org/10.3389/fcimb.2017.00358
- Gal Y., Marcus H., Mamroud E., Aloni-Grinstein R. Mind the gap — a perspective on strategies for protecting against bacterial infections during the period from infection to eradication. Microorganisms. 2023;11(7):1701. DOI: https://doi.org/10.3390/microorganisms11071701
- Granger V., Peyneau M., Chollet-Martin S., de Chaisemartin L. Neutrophil extracellular traps in autoimmunity and allergy: immune complexes at work. Front. Immunol. 2019;10:2824. DOI: https://doi.org/10. 3389/fimmu.2019.02824
- Jönsson F., Mancardi D.A., Albanesi M., Bruhns P. Neutrophils in local and systemic antibody-dependent inflammatory and anaphylactic reactions. J. Leukoc. Biol. 2013;94(4):643–54. DOI: https://doi.org/10.1189/jlb.1212623
- Tang A.H., Brunn G.J., Cascalho M., Platt J.L. Pivotal advance: endogenous pathway to SIRS, sepsis and related conditions. J. Leukoc. Biol. 2007;82(2):282–5. DOI: https://doi.org/10.1189/jlb.1206752
- Lee-Lewis H., Anderson D. Absence of inflammation and pneumonia during infection with non-pigmented Yersinia pestis reveals new role for the pgm locus in pathogenesis. Infect. Immun. 2010;78(1):220–30. DOI: https://doi.org/10.1128/IAI.00559-09
- Шмелькова Т.П., Кравцов А.Л., Щуковская Т.Н. и др. Влияние биологических свойств чумного микроба на развитие апоптоза лейкоцитов крови человека в системе in vitro. Проблемы особо опасных инфекций. 2007;(1):85–9. Shmelkova T.P., Kravtsov A.L., Shchukovskaya T.N., et al. Effects of Yersinia pestis biologic characteristics on the development of human human blood leukocyte apoptosis in the in vitro system. Problems of Particularly Dangerous Infections. 2007;(1):85–9. EDN: https://elibrary.ru/icabrv
- Кравцов А.Л., Бугоркова С.А., Клюева С.Н. и др. Оценка изменений фенотипа, интенсивности дегрануляции, гибели и лизиса нейтрофилов при моделировании ex vivo стафилококковой бактериемии. Журнал микробиологии, эпидемиологии и иммунобиологии. 2023;100(4):293–305. Kravtsov A.L., Bugorkova C.A., Klyueva S.N., et al. Assessment of changes in the phenotype, intensity of degranulation, death and lysis of neutrophils in ex vivo modeling of Staphylococcal bacteriemia. Journal of Microbiology, Epidemiology and Immunobiology. 2023;100(4):293–305. DOI: https://doi.org/10.36233/0372-9311-384 EDN: https://elibrary.ru/qgughr
- Vera E.J., Chew Y.V., Nicholson L., et al. Standartization of flow cytometry for whole blood immunophenotyping of islet transplant and transplant clinical trial recipients. PLoS One. 2019;14(5):e0217163. DOI: https://doi.org/10.1371/journal pone.0217163
- Bassøe C.F., Solberg C.O. Phagocytosis of Staphylococcus aureus by human leukocytes: quantitation by a flow cytometric and a microbiological method. Acta Pathol. Microbiol. Immunol. Scand. C. 1984;92(1):43–50. DOI: https://doi.org/10.1111/j.1699-0463.1984.tb00050.x
- Källquist L., Hansson M., Persson A.M., et al. The tetraspanin CD63 is involved in granule targeting of neutrophil elastase. Blood. 2008;112(8):3444–54. DOI: https://doi.org/10.1182/blood-2007-10-116285
- Zeng W., Song Y., Wong R., et al. Neutrophil elastase: From mechanisms to therapeutic potential. J. Pharm. Anal. 2023;13(4):335–66. DOI: https://doi.org/10.1016/j.jpha.2022.12.003
- Weinrauch Y., Drujan D., Shapiro S.D., et al. Neutrophil elastase targets virulence factors of enterobacteria. Nature. 2002;417(6884):91–4. DOI: https://doi.org/10.1038/417091a
- Shi J., Gantz T. The role of protegrins and other elastase-activated polypeptides in the bactericidal properties of porcine inflammatory fluids. Infect. Immunity. 1998;66(8):3611–7. DOI: https://doi.org/10.1128/iai.66.8.3611-3617.1998
- Papayannopoulos V., Metzler K.D., Hakkim A., Zychlinsky A. Neutrophil elastase and myeloperoxidase regulate the formation of neutrophil extracellular traps. J. Cell Biol. 2010;191(3):677–91. DOI: https://doi.org/10.1083/jcb.201006052
- Kravtsov A.L., Grebenyukova T.P., Bobyleva E.V., et al. Flow cytofluorometric assay of human whole blood leukocyte DNA degradation in response to Yersinia pestis and Staphylococcus aureus. In: Proceedings of Saratov Fall Meeting 2001: Optical Technologies in Biophysics and Medicine. Volume 4241. Saratov;2001:260–7. DOI: https://doi.org/10.1117/12.431530
- Traganos F., Darzynkiewicz Z. Lysosomal proton pump activity: supravital cell staining with acridine orange differentiates leukocyte subpopulations. Methods Cell Biol. 1994;41:185–94. DOI: https://doi.org/10.1016/s0091-679x(08)61717-3
- Abrams W.R., Diamond L.W., Kane A.B. A flow cytometric assay of neutrophil degranulation. J. Histochem. Cytochem. 1983;31(6):737–44. DOI: https://doi.org/10.1177/31.6.6404983
- Montminy S.W., Khan N., McGrath S., et al. Virulence factors of Yersinia pestis are overcome by a strong lipopolysaccharide response. Nat. Immunol. 2006;7(10):1066–73. DOI: https://doi.org/10.1038/ni1386
- Owen C.A., Campbell M.A., Sunnes P.L., et al. Cell surface-bound elastase and cathepsin G on human neutrophils: a novel, non-oxidative mechanism by which neutrophils focus and preserve catalytic activity of serine proteases. J. Cell Biol. 1995;131(3):775–89. DOI: https://doi.org/10.1083/jcb.131.3.775
- Landoni V.I., Chiarella P., Martire-Greco D., et al. Tolerance to lipopolysaccharide promotes an enhanced neutrophil extracellular traps formation leading to a more efficient bacterial clearance in mice. Clin. Exp. Immunol. 2012;168(1):153–63. DOI: https://doi.org/10.1111/j.1365-2249.2012.04560.x
- Кравцов А.Л., Гончарова А.Ю., Бугоркова С.А. и др. Формирование нейтрофильных внеклеточных ловушек при моделировании чумной инфекции у мышей, иммунизированных Yersinia pestis EV НИИЭГ. Проблемы особо опасных инфекций. 2020;(4):70–4. Kravtsov A.L., Goncharova A.Yu., Bugorkova S.A., et al. Formation of neutrophil extracellular traps when modeling plague infection in mice immunized with Yersinia pestis EV NIIEG. Problems of Particularly Dangerous Infections. 2020;(4):70–4. DOI: https://doi.org/10.21055/0370-1069-2020-4-70-74 EDN: https://elibrary.ru/ovzjoe
- Khodoun M.V., Strait R., Armstrong L., et al. Identification of markers that distinguish IgE- from IgG-mediated anaphylaxis. Proc. Natl. Acad. Sci. USA. 2011;108(30):12413–8. DOI: https://doi.org/10.1073/pnas.1105695108
Supplementary files