Stability of vaccine strains of seasonal live attenuated influenza vaccines when adapted to MDCK cell culture
- Authors: Matyushenko V.A.1, Kostromitina A.D.1, Stepanova E.A.1, Rudenko L.G.1, Isakova-Sivak I.N.1
-
Affiliations:
- Institute of Experimental Medicine
- Issue: Vol 102, No 3 (2025)
- Pages: 296-309
- Section: ORIGINAL RESEARCHES
- URL: https://microbiol.crie.ru/jour/article/view/18876
- DOI: https://doi.org/10.36233/0372-9311-669
- EDN: https://elibrary.ru/PCCKFR
- ID: 18876
Cite item
Abstract
Introduction. Currently, the vast majority of influenza vaccines in the world are produced using developing chicken embryos as substrate, but there is an urgent necessity for transferring vaccine production to continuous cell lines, which would ensure uninterrupted production during an avian influenza pandemic and also allow the vaccine to be administered to individuals with chicken protein allergies. When vaccine strains of live attenuated influenza vaccine (LAIV) grow in mammalian cells, adaptation mutations can occur that may affect the antigenic and immunogenic properties of the vaccine.
The aim of the study is to investigate the biological properties of vaccine strains of LAIV subtypes A/H1N1 and A/H3N2, produced by the classical reassortment in eggs, when adapted to Madin–Darby canine kidney (MDCK) cell culture.
Materials and methods. In current study, LAIV strains A/17/California/2009/38 (H1N1pdm09) and A/17/Texas/12/30 (H3N2) were used. These viruses were passaged on MDCK 5 times and the growth properties of the isolated clones by the plaque assay were analyzed in vitro and in vivo, also immunogenicity, cross-reactivity and protective efficacy were estimated on a mouse model, as well as using hyperimmune rat sera. Experimental series of LAIV strains A/17/Bolivia/2013/6585 (H1N1), A/17/Switzerland/2013/1 (H3N2) and B/60/Phuket/2013/26 were produced on MDCK cells at the Vector State Research Center of Virology and Biotechnology. The surface protein genes of monovalent vaccines were sequenced, and the mutations in HA and NA were identified and compared between adaptation to MDCK culture in laboratory and industrial conditions.
Results. Sequencing of surface antigens of MDCK-adapted variants of the A/H1N1 virus revealed adaptation mutations in the hemagglutinin molecule N156D (HA1 subunit) and A44V (HA2 subunit), which enhanced the replicative properties of the H1N1 vaccine strain in MDCK cells. The study of this MDCK-adapted variant in a mouse experiment showed no effect of the detected mutations on the immunogenic and protective properties of the vaccine. Adaptation of the H3N2 vaccine strain to MDCK cells resulted in a significantly higher number of substitutions in the HA molecule compared to the H1N1 virus, and it was shown that the Y85E and N154K mutations in HA2 are critical for virus multiplication in cell culture, and the set of mutations P215T in HA1 and W92G, D160H in HA2 gave the vaccine strain a significant advantage for growth in MDCK cells, which can be effectively used in the production of cell-based LAIVs.
Discussion. The study of the MDCK cell-produced series of LAIVs showed the presence of adaptation mutations in the hemagglutinin molecule of the H1N1 (K116E in the HA2 subunit) and H3N2 (S219Y and N246K in the HA1 subunit) strains. It is important to note that all the adaptation mutations studied did not affect the antigenicity of the vaccine strains.
Conclusion. In general, the data obtained in the course of the study indicate the feasibility of producing a culture-based live attenuated influenza vaccine from vaccine strains prepared by classical reassortment in eggs.
Full Text
Introduction
Annual vaccination against seasonal influenza is the most effective way to combat this infection [1]. For over 70 years, the allantoic fluid of the embryonated chicken eggs has been recognized as the most optimal substrate for receiving of high-yield virus material, which made it possible to produce a sufficient number of vaccine doses for seasonal flu vaccine campaign [2, 3]. However, the outbreak of highly pathogenic H5N1 avian influenza in Hong Kong in 1997, and since 2003, the widespread spread of this infection throughout the world, forced the scientific community to consider switching the production of influenza vaccines to immortalized cell lines, since such production would not depend on the promptly supply of embryonated chicken eggs in the avian influenza presence [4]. Furthermore, the production of vaccine viruses in cell culture allows avoiding the occurrence of egg-adaptation mutations in vaccine strains, which could have a negative impact on the antigenicity and immunogenicity of the vaccine and, as a result, reduce its protection effectiveness [5, 6]. Generally accepted cell line for the influenza vaccines production is the Madin-Darby canine kidney (MDCK) cell culture, which is currently used to produce the FluCellVax — cultural inactivated influenza vaccine [7]. Another important advantage of the culture influenza vaccine is the possibility of its use in people suffering from an egg allergy.
The preparation of vaccine strains for a Russian licensed live attenuated influenza vaccine (LAIV) is currently possible only by classical reassortment in embryonated chicken eggs, in which the 6:2 vaccine formula is obtained according to a proven protocol and usually allows obtaining the required vaccine strain [8]. To transfer LAIV production from chicken eggs to MDCK cell culture, studies were previously conducted to obtain vaccine strains in MDCK cells. It was shown that during classical reassortment in this cell line of the epidemic virus and the attenuation donor, there was no formation of a vaccine strain with the required 6:2 genome formula [9]. Since 2019, the World Health Organization has divided strains for cell-based and egg-based influenza vaccines in its recommendations for current influenza virus strains for seasonal influenza vaccines because of the fact that many studies have shown that strains isolated on the same substrate should be used for vaccine production in order to avoid the appearance of adaptive mutations [10]. The issue of obtaining LAIV strains in MDCK cells could be resolved using reverse genetics methods to assemble influenza viruses with a given set of genes, however, the presence of a patent for this technology by MedImmune excludes the possibility of its use for commercial production [11]. Thus, one of the options for obtaining culture LAIV is the use of vaccine strains obtained by classical reassortment in developing chicken embryos for their growth on a cell line. Since the substrate for the accumulation of vaccine viruses is exchanged, it is necessary to study the stability of the main biological properties of LAIV strains during their adaptation to MDCK cells.
The aim of this study was to identify possible adaptation mutations in the LAIV strains A/H1N1 and A/H3N2 obtained by the classical reassortment method in the emryonated chicken eggs during their adaptation to the MDCK cells, with subsequent assessment of the effect of the detected mutations on the growth characteristics of the viruses, their immunogenicity, cross-reactivity and protective activity in the experiment. Furthermore, as part of the study, an experimental series of cultural LAIV produced by the State Research Center of Virology and Biotechnology Vector on MDCK cell culture using industrial bioreactors was analyzed [12].
Materials and methods
Viruses
The LAIV strains A/17/California/2009/38 (H1N1pdm09) (Calif17) [13] and A/17/Texas/12/30 (H3N2) (Tex17) [14] were used, the surface genes of which corresponded to the epidemic strains A/California/07/2009 (H1N1pdm09) (NCBI database number: NC_026433 (HA) and NC_026434 (NA)) and A/Texas/50/2012 (H3N2) (NCBI database number: KC892248 (HA) and KC892237 (NA)) respectively. Mouse-adapted influenza virus A/California/07/09 (H1N1) was obtained from the Collection of Influenza and ARVI Viruses of the A.A. Smorodintsev Research Institute of Influenza and were used for the challenge experiment [15]. Experimental series of LAIV strains A/17/Bolivia/2013/6585 (H1N1), A/17/Switzerland/2013/1 (H3N2) and B/60/Phuket/2013/26 were produced on the MDCK cells at the Vector State Research Center of Virology and Biotechnology using bioreactors with a culture vessels volume of 2 liters (Multigen) and 10 liters (Biostat) [12].
Virus growth in eggs and MDCK cells and infectious titer counting
To grow influenza viruses in eggs, 10–11-day-old embryonated chicken eggs were infected with 0.2 ml of viral liquid, after which the eggs were incubated for 48 h at 33°C. Virus propagation in MDCK cells was carried out on a 24-hour monolayer with 90–95% cells confluence, grown in DMEM with 1× antibiotic-antimycotic (AA) (Gibco) and 10% fetal bovine serum (FBS) (Biolot) at 37°C in a incubator with 5% CO2. To infect MDCK cell culture, the monolayer was washed twice with a warm solution of phosphate-buffered saline (PBS), after which the viral suspension was added in a volume of 1, 2, 4 ml to T-25, T-75 and T-175 flasks, respectively. After contact for 1 h at 33°C and 5% CO2, the inoculum was removed and condition medium (DMEM with 1×AA and 1 μg/ml TPCK trypsin (Sigma-Aldrich)) was added. After 72 h of incubation at 33°C, the cytopathic effect of the virus was visually assessed and its titer was counted in the hemagglutination assay using the standard method with chicken RBC. Infectious titers of viruses in both cultivation systems were determined by the limiting dilution assay. The titer in MDCK cells was evaluated at 96-well plates with a daily monolayer, while serial 10-fold dilutions were prepared in condition medium. After 1 h adsorption at 33°C, the inoculum was removed, the cells were washed and then incubated in a maintenance medium for 3 days at 33°C and 5% CO2. The presence of viruses in the wells was determined in a hemagglutination assay with chicken RBC. Viral titers in eggs and MDCK cells were counted using the Reed and Mench method [16] and put as 50% embryonated or tissue culture infectious doses (lgEID50/ml and lgTCID50/ml).
Virus adaptation to MDCK cells
Adaptation of influenza viruses to MDCK cell culture was performed over 5 serial viral passages at an optimal multiplicity of infection (MOI) of 0.001–0.010, followed by virus cloning using the plaque assay. For this purpose, 10-fold dilutions of viruses were applied in double replicates to 6-well plates seeded with MDCK cells the day before. After an hour of contact with regular plates shaking, the inoculum was removed and 3 ml of an agar coating obtained by mixing equal volumes of 2×DMEM medium (in the presence of 2×AA and 2 μg/ml TPCK trypsin) and 1.6% low-melting agarose (Lonza) were added to the wells. On the 3rd–5th day of incubation, the viral plaques were visually observed, 20–30 plaques that were easily separated from each other were isolated at limiting dilutions, separate clones of the virus was isolated from each plaque, which was then grew on the MDCK cell culture. Each propagated viral clone was whole-genome sequenced by the Sanger method using the BigDye Terminator Cycle Sequencing Kit v3.1 (Thermo). First of all, the presence of unique attenuating mutations of LAIV strains was checked, since it is their existence that determines the attenuating of LAIV and the possibilities of its use [17], and then a search was conducted for amino acid substitutions in the genes of surface proteins: hemagglutinin (HA) and neuraminidase (NA).
Animal experiments
In animal experiments, CBA mice (Stolbovaya, Russia) were used. The study was approved by the Ethics Committee of the Institute of Experimental Medicine (protocol No. 1/20 dated 02/27/2020). To assess the immunogenicity and protective efficacy of the H1N1 vaccine strains, female CBA mice were immunized intranasally at a dose of 106 TCID50 in a 50 μl volume , twice with a difference of 3 weeks, after which, after another 21 days, blood serum was collected to assess antibody levels in the hemagglutination inhibition assay (HAI) and enzyme-linked immunosorbent assay (ELISA) using a standard methods. To study the protective efficacy, an experiment was carried out on mice immunized according to the scheme described above, followed by infection with a lethal dose 5.0 lg EID50of the mouse-adapted A/California/07/09 (H1N1) strain with daily monitoring of survival for 14 days. To assess the cross-reactivity of antibodies produced to the H3N2 LAIV strains, hyperimmune rat sera were obtained. For this purpose, Wistar rats (Rappolovo, Russia) were immunized 5 times with an interval of 5–7 days. The first, third and fifth immunizations were administered intraperitoneally in a volume of 5 ml/animal, the second and fourth immunizations were administered subcutaneously in the withers using complete Freund's adjuvant in a volume of 1 ml/rat, the ratio of virus and adjuvant was 1 : 1. A week after the last immunization, whole blood samples were taken from all immunized animals. After centrifugation of the blood for 15 min at 3000g, the serum was carefully collected, and aliquots were stored at –20°C.
Immunological methods
The animal blood serum was studied in HAI according to the standard WHO protocol with chicken RBC and treatment of the serum with a receptor-destroying enzyme (Denka). The serum titer in HAI was counted as the last dilution at which complete inhibition of erythrocyte agglutination was observed.
ELISA with mouse serum samples was performed using the relevant wild influenza viruses purified on a sucrose density gradient as the antigen. The 16 agglutinating units (AU) of antigen were added to 96-well plates with high sorption (Corning) 50 μl/well and incubated overnight at 4°C. The plates were washed 3 times with washing buffer (PBS + 0.05% Tween-20 (Biolot)), unbound sites were blocked with 1% bovine serum albumin. Two-fold dilutions of sera were prepared in separate U-bottom plates, which were then transferred to the wells of the ELISA plate washed from the blocking solution. After incubation for 1 h at 37°C, the plates were washed 3 times with washing buffer, dried, and secondary antibodies conjugated with horseradish peroxidase, anti-mouse IgG were added in dilution ration 1 : 10,000. The plates were incubated for 1 h at 37°C, washed 5 times with washing buffer, dried, and 50 μl/well of TMB substrate (Thermo) were added, which was incubated in the dark for up to 20 min at room temperature. The reaction was stopped by adding 50 μl of 1 M H2SO4. The primary ELISA results were recorded on a spectrophotometer (Bio-Rad) at a wavelength of 450 nm. The area under the curve parameter of optical density was calculated using the GraphPad Prizm v. 7 software package.
Statistical data analysis
Statistical processing was performed using the GraphPad Prizm v. 7 software. For pairwise comparison of virus titers, the nonparametric Mann-Whitney U-test was used; antibody levels between groups of immunized mice were compared in a nonparametric one-way ANOVA with the Kruskal-Wallis correction. Differences were considered significant at p < 0.05.
Results
Adaptation of the H1N1 vaccine strain to MDCK cells in laboratory conditions
As a result of serial passaging of the Calif17 vaccine strain in MDCK cell culture with subsequent cloning by the plaque method, 21 virus variants were obtained. Sequencing showed the safeguarding of unique attenuating mutations in the genes of internal and non-structural proteins. At the same time, only 2 of the 21 studied variants did not have amino acid substitutions in the HA molecule, and in the remaining isolates, either N156D mutations in HA1, or A44V in HA2, or both were detected simultaneously (Table 1).
Table 1. Mutations found in the HA molecule of MDCK-adapted variants of the Calif17 vaccine strain
HA subunit | Amino acid position | Original virus Calif17 | MDCK-adapted viral variants | ||
Calif17-1 (9 clones) | Calif17-4 (7 clones) | Calif17-8 (3 clones) | |||
HA1 | 156 | Asn | Asp | Asn | Asp |
HA2 | 44 | Ala | Ala | Val | Val |
The arrangement of amino acid substitutions in the HA molecule of Calif-17 cell clones is shown in Fig. 1.
Fig. 1. Mapping of adaptation amino acid substitutions in the HA molecule of the vaccine strain Calif17.
The arrangement of amino acids is shown on the HA monomer A/California/04/2009 (H1N1) (PDBID: 3UYX). Illustrations were obtained using the «RasMol v. 2.7.5» program.
The growth capacity of three MDCK-adapted variants (Calif17-1, Calif17-4, and Calif17-8) with different sets of found mutations were studied in eggs and MDCK cells in comparison with the original virus propagated in eggs (Calif17). Reproduction of the original Calif17 vaccine strain on different substrates also differed by almost two orders of magnitude: the virus titer in eggs was 8.0 lg EID50/ml, while the virus titer in MDCK cells was 6.3 lg TCID50/ml (Fig. 2). In the study of MDCK-adapted variants of the Calif17 strain, a reliable increase in virus titers in MDCK cell culture by more than 10 times was found in 2 strains (Calif17-4 — 7.3 lg TCID50/ml and Calif17-8 — 7.6 lg TCID50/ml), both containing the A44V mutation in HA2. The Calif17-8 variant also retained a high level of reproduction in embryonated chicken eggs (8.2 lg EID50/ml), while the Calif17-1 strain, which has only the N156D mutation in HA1, did not improve reproduction in cell culture and decreased it in eggs by more than 30 times (6.2 lg TCID50/ml and 6.6 log EID50/ml). Thus, the A44V mutation in HA2 has a positive effect on the replication of the H1N1pdm09 vaccine strain in both culture systems.
Fig. 2. Infectious titers of the LAIV strain A/17//California/2009/38 (H1N1pdm09) and its MDCK-adapted variants in embryonated chicken eggs and MDCK cells.
*p < 0.05 compared with TCID50/ml Calif17; †p < 0.05 compared with EID50/ml Calif17.
The isolated variants of the Calif17 virus after plaque cloning, carrying one of the two mutations, acquired both mutations during subsequent accumulation in the MDCK cell — A44V in HA2 and N156D in HA1, becoming identical in amino acid composition to the Calif17-8 variant. This phenomenon suggests that these two mutations are strongly associated with the adaptation of the virus to the mammalian cell line, but the initial five-times passaging did not completely replace the corresponding amino acids in the heterogeneous virus population. Additional growing of variants with one mutation in the MDCK cells continued the process of virus adaptation, introducing the missing mutation in the HA gene. Thus, in the experiment on the immunogenicity and protective activity of viruses in mice, it was possible to compare only the Calif17-8 strain, carrying both adaptation mutations, with the original Calif17 virus propagated in eggs.
Figure 3 shows the results of ELISA of blood serum from immunized mice, where the epidemic strain A/California/09/07 (H1N1pdm09), grew in the eggs and purified on a sucrose density gradient, served as an antigen substrate. Statistical processing of the experimental data showed that there are no significant differences between levels of IgG antibodies induced by both vaccine strains, which indicates the absence of a negative effect of the detected adaptation mutations A44V in HA2 and N156D in HA1 on the immunogenicity of LAIV H1N1pdm09.
Fig. 3. Immunogenicity and protective efficacy of the H1N1pdm09 vaccine strain obtained in the embryonated chicken eggs and its analogue adapted to the MDCK cell culture in an experiment on CBA mice.
a — dependence of optical density on serum dilution in ELISA; b — calculation of the area under the curve according to the data of graph a; c — survival rate of immunized and control mice after experimental infection with the lethal virus A/California/09/07 MA.
Statistical analysis was performed by the method of nonparametric one-way ANOVA with the Kruskal–Wallis correction.
The cross-reactivity of antibodies induced by the MDCK-adapted variant of Calif17-8 and the vaccine strain Calif17 was assessed in HAI using the classical method. Adaptation mutations did not affect the ability of the produced antibodies to bind the original HA variant of the A/California/07/09 (H1N1pdm09) strain (Table 2), which is completely consistent with the immunogenicity data presented above.
Table 2. Cross-reactivity of antibodies produced in response to immunization of mice with different variants of LAIV H1N1pdm09
Antigens | HAI titer of antibodies in blood sera of mice vaccinated with the H1N1 viral variants | |
Calif17 | Calif17-8 | |
Calif-wt | 640 | 320 |
Calif17 | 640 | 320 |
Calif17-8 | 320 | 320 |
The effect of the adaptation mutations N156D in HA1 and A44V in HA2 on the protective efficacy was studied using the wild virus A/California/07/09 (H1N1pdm) adapted to mice. In the challenge experiment, mice immunized with the vaccine strains Calif17 and Calif17-8, as well as the control group of naive animals, were infected with the mouse-adapted lethal virus at a dose of 105 lgEID50, after which daily survival monitoring have been carrying out for 14 days. The protective efficacy of both the egg-derived LAIV strain and its MDCK-adapted variant was 100%, while the animals of the control group died completely, and the survival rate in it was 0% (Fig. 3, c, d). Thus, the studied MDCK adaptated mutations did not affect the protective efficacy of the LAIV strain Calif17.
Adaptation of the H3N2 vaccine strain to MDCK cells in laboratory conditions
The vaccine strain A/17/Texas/12/30 (H3N2) (Tex17) containing HA and NA from the epidemic influenza virus A/Texas/50/2012 (H3N2) was used in the study. After adaptation of Tex17 to the MDCK cell culture, 20 clones of Tex17 were isolated, 10 of which were found to have various amino acid differences in the HA molecule during sequencing (Table 3).
Table 3. Mutations found in the HA molecule of MDCK-adapted variants of the Tex17 vaccine strain
HA Subunits | Amino acid position | Original virus | MDCK-adapted variants | |||||||||
Тех17-1 | Тех17-4 | Тех17-8 | Тех17-9 | Тех17-11 | Тех17-15 | Тех17-16 | Тех17-17 | Тех17-20 | Тех17-21 | |||
HA1 | 176 | Val | Val | Val | Ile | Ile | Val | Val | Ile | Val | Val | Ile |
215 | Pro | Pro | Pro | Pro | Pro | Thr | Thr | Pro | Thr | Pro | Pro | |
221 | Pro | Pro | Pro | Ser | Ser | Pro | Pro | Ser | Pro | Pro | Ser | |
265 | Asp | Asp | Asp | Asp/ Glu | Asp/ Glu | Asp/ Glu | Asp/ Glu | Asp/ Glu | Asp | Asp | Asp | |
301 | Arg | Arg | Arg | Arg | Arg | Arg | Arg | Arg | Arg | Lys | Arg | |
HA2 | 79 | Asp | Asp | Asp | Asp | Gly | Asp | Asp | Asp | Asp | Asp | Asn |
83 | Tyr | His | Tyr | Tyr | Tyr | Tyr | Tyr | Tyr | Tyr | Tyr | Tyr | |
85 | Glu | Glu | Glu | Asp | Glu | Glu | Glu | Glu | Glu | Glu | Glu | |
92 | Trp | Trp | Trp | Trp | Trp | Trp | Trp | Trp | Trp/Gly | Trp | Trp | |
124 | Lys | Lys | Glu | Lys | Lys | Lys | Lys | Lys | Lys | Lys | Lys | |
154 | Asn | Asn | Asn | Asn | Asn | Asn | Asn | Lys | Asn | Asn | Asn | |
160 | Asp | Asp | Asp | Asp | Asp | Asp | Asp | Asp | His | Asp | Asp | |
169 | Asn | Asn | Asn | Asn | Asn | Asn | Lys | Asn | Asn | Asn | Asn | |
Note: MDCK-adapted amino acid substitutions in HA have been highlighted compared to the egg-derived Tex17 vaccine strain.
No matching mutations were found in the HA molecule of MDCK-adapted clones of the vaccine strain Tex17, but frequently occurring amino acid substitutions were noted: V176I, P215T, P221S and D265E in HA1. Single mutations were also identified: R301K in HA1, D79N, D79G, Y83H, E85D, W92G, K124E, N154K, D160H and N169K in HA2 (Table 3). The localization of frequently occurring and single mutations is different: the former are located in the globular part of HA near the receptor-binding site, the latter are in the HA stalk-domain.
An examination of the vaccine strain reproduction showed that the original vaccine strain Tex17 reproduces 50 times better in the eggs than in the MDCK cells. Interestingly, one of the MDCK-adapted variants, strain Tex17-16, showed the most significant increase in infectious titer in MDCK cells compared to the egg-derived vaccine strain Tex17 (Fig. 4). Thus, the set of mutations V176I, P221S, D265E in HA1 and N154K in HA2 is associated with an increase in the reproductive capacity of the vaccine strain in MDCK cell culture.
Fig. 4. Reproduction of influenza A/17/Texas/12/30 (H3N2) vaccine viruses in the different culture systems.
*p < 0.05 compared with TCID50/ml Tex17; †p < 0.05 compared with EID50/ml Tex17-17.
Furthermore, the variant Тех17-8 was identified, which had a significantly lower titer in the MDCK cell culture compared to the control strain Тех17, which was affected by the amino acid substitutions P221S, D265E in HA1 and Y85E in HA2. Thus, it follows that the N154K and Y85E mutations in HA2 have critical for virus replication in cell culture and require further study. The strain Тех17-17, which replicated 200 times better in the MDCK cell culture than in the developing chicken embryo system, also turned out to be interesting. This means that the adaptation mutations P215T in HA1 and W92G, D160H in HA2 gave the vaccine strain a significant advantage for replication in the MDCK cell culture, which can be effectively used in the production of cell-based LAIV. However, the set of the specified mutations significantly reduced the reproduction of viruses in the eggs, and if we pay attention to the viruses Tex17-11 and Tex17-15, we can see that these variants differ only in mutations in the HA2 subunit of the HA molecule, and it is the amino acid differences in the HA stalk-domain that are key in the adaptation of H3N2 vaccine strains to the MDCK cells.
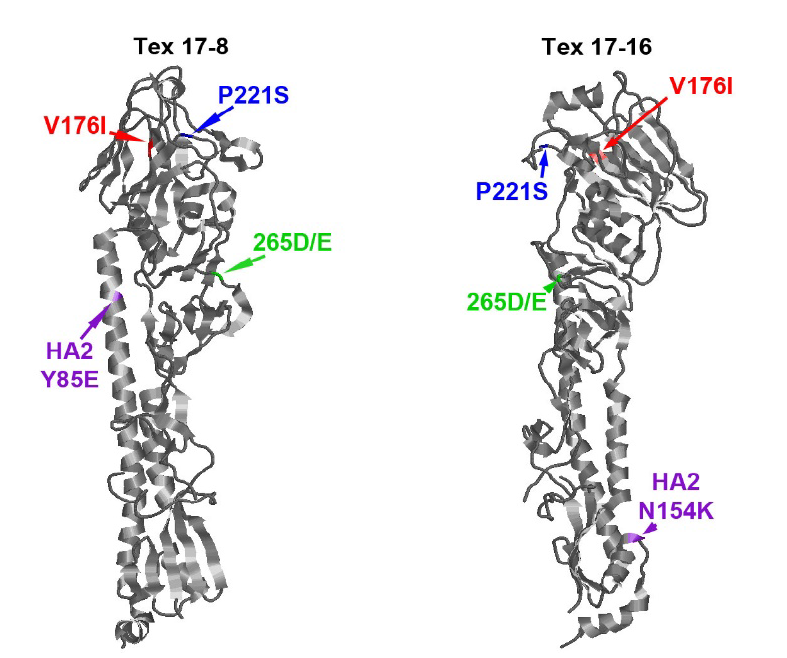
Figure 5 shows the three-dimensional structures of the HA molecules of the vaccine strains Tex17-8 and Tex17-16, on which the noticed adaptation mutations are marked. It is evident that the mutations that critically affected the level of reproduction of vaccine viruses in the MDCK cells are located in the HA stalk-domain. It is also of interest to study the immunogenicity and antigenicity of these viruses, but current influenza viruses of the H3N2 subtype are not able to infect mice, therefore, within the framework, study of the immunogenicity of H3N2 viruses was not carried out in a mouse model. To assess the antigenicity of the most interesting MDCK-adapted variants, hyperimmune rat sera were obtained.
Fig. 5. Mapping of adaptation amino acid substitutions in the HA molecule of the vaccine strain Tex17.
The arrangement of amino acids is shown on the HA monomer of A/Pennsylvania/14/2010 (H3N2) (PDBID: 6MZK). Illustrations were obtained using the «RasMol v. 2.7.5» program
The cross-reactivity of antibodies induced by the cell clones Tex17-8, Tex17-16 and Tex17-17 was assessed in HAI using the classical method. It was shown that adaptation mutations did not affect the ability of the produced antibodies to bind the HA, of the egg-derived A/Texas/50/2012 (H3N2) strain (Table 4).
Table 4. Cross-reactivity of antibodies in hyperimmune rat sera obtained to different variants of the LAIV H3N2 vaccine strain
Antigens | HAI titer of antibodies in hyperimmune sera of rats obtained to the indicated variants of the vaccine virus | |||
Тех17 | Тех17-8 | Тех17-16 | Тех17-17 | |
Тех-wt | 1280 | 320 | 640 | 640 |
Тех17 | 1280 | 320 | 320 | 1280 |
Тех17-8 | 2560 | 320 | 320 | 1280 |
Тех17-16 | 640 | 640 | 640 | 640 |
Тех17-17 | 1280 | 320 | 640 | 640 |
Adaptation of trivalent LAIV vaccine strains to MDCK cell culture under industrial production conditions
In Russia, cultured LAIV is being developed at the State Research Center of Virology and Biotechnology Vector, using reassortant LAIV vaccine strains prepared by the classical reassortment method at the developing chicken embryos as the starting material. The company registered a system for producing LAIV in mammalian cell culture and successfully produced an experimental series of cellular monovalent vaccines against seasonal influenza viruses in 2015 [12] and then conducted phase I clinical trials [18]. However, it remained unknown how the production process affected the properties of the LAIV strains. Sequencing of the HA and NA surface protein genes of cellular monovalent vaccines showed that adaptation mutations appeared only in the HA molecules of influenza A viruses, while no amino acid substitutions were found in the B/60/Phuket/2013/26 strain (Table 5). Thus, in the vaccine strain A/17/Bolivia/2013/6585 (H1N1pdm09), the K116E mutation in the HA2 subunit was identified, and in the strain A/17/Switzerland/2013/1 (H3N2), the S219Y and N246K mutations in the HA1 subunit were identified.
Table 5. Amino acid substitutions in surface antigens of experimental cellular monovalent LAIV
Vaccine | Gene | Protein | Amino acid | Original vaccine strain | Vaccine strain after production passages |
A/17/Bolivia/2013/6585 (H1N1pdm) | HA | НА2 | 116 | Lys | Glu |
NA | NA | Mutation not found | |||
A/17/Switzerland/2013/1 (H3N2) | HA | HA1 | 219 | Ser | Tyr |
246 | Asn | Lys | |||
NA | NA | Mutation not found | |||
B/60/Phuket/2013/26 | HA | НА | Mutation not found | ||
NA | NA | Mutation not found | |||
In Fig. 6, the positions at which amino acid substitutions were detected during adaptation of vaccine strains to cell culture on a laboratory scale (A44V in HA2 of the H1N1 subtype, V176I, P215T, P221S and D265E in HA1 of the H3N2 subtype) and during the production of culture LAIV batches (K116E in HA2 of the H1N1 subtype, S219Y and N246K in HA1 of the H3N2 subtype) are highlighted on the monomers of the corresponding HA molecules. It should be noted that, although the mutations detected are not identical in different viruses, their common localization can be observed in each subtype. Thus, positions 44 and 116 in HA2 of the H1N1 subtype are in close proximity to each other, positions 176, 215, 219, 221 in HA1 of the H3N2 subtype are localized in the region of the receptor-binding site.
Fig. 6. Mapping of adaptation amino acid substitutions in the HA molecule of the vaccine strains Calif17 and Bolivia17 (a), Tex17 and Switzerland17 (b).
The arrangement of amino acids is shown on the HA monomer of A/California/04/2009 (H1N1) and A/Singapore/H2011.447/2011 (H3N2) (PDBID: 3UYX and 4WEA, respectively). Illustrations were obtained using the «RasMol v. 2.7.5» program.
Discussion
Adaptation of the virus to a new host range inevitably entails the emergence of adaptive mutations, which can lead to changes in the properties of the original virus. In this case, adaptive mutations can be dramatic, as, for example, occurred during the adaptation of influenza viruses from avian cells to mammalian cells, which led to the H2N2 influenza pandemics in 1957 and H3N2 in 1968 [19–22]. The substrate for the production of biomass for obtaining an influenza vaccine, both live and inactivated, can also affect its properties. As mentioned above, the preparation of strains for Russian LAIV is possible only in the embryonated chicken eggs, while there are known cases of the emergence of egg-adaptive mutations that affected the antigenicity of the vaccine strain, which led to a decrease in the effectiveness of the vaccine during its mass use [21, 23–25]. Since A/H3N2 strains are the most variable and more susceptible to antigenic drift than others, this circumstance must be taken into account when producing vaccine viruses in various culture substrates [21]. Thus, from 2013 to 2018, a number of mutations were discovered that critically affected the antigenicity of circulating viruses: the F159Y and K160T substitutions in antigenic site B, together with the N residue in site 158, contribute to the acquisition of an additional glycosylation site, which actively helps the virus evade the immune response [26–28]. Then, in the process of evolution, a characteristic amino acid substitution N171K occurred, located on the antigenic site D of the HA molecule, as well as the D122N and T135K substitutions in antigenic site A, each of which causes the loss of N-linked glycosylation sites [29]. The following season revealed the presence of a S144K substitution in the HA1 molecule, which is located in the antigenic site flanking the receptor-binding site. Two clusters of the H3N2 influenza virus showed that the I58V and S219Y substitutions, as well as the 122D and S262N substitutions, which lead to the loss of the glycosylation site, are also antigenically important [21]. In the current study, during adaptation to MDCK cells, mutations were found that are also probably located in antigenic sites: V176I, P215T, P221S and S219Y, however, it was shown that they do not affect the antigenicity of the vaccine strain, but affect its ability to grow in mammalian cells.
Studies of the infectious activity and stability of high-yielding influenza virus strains for inactivated influenza vaccine demonstrated that cultivation of H1N1 and H3N2 influenza viruses in Vero or MDCK cell culture under acidified conditions maintains virus stability, which was successfully used in the production of inactivated influenza vaccine against H5N1 avian influenza. Passaging of viruses without additional conditions contributed to the emergence of adaptive mutations N50K (H1N1) and D160E (H3N2) in the HA2 molecule, which improved viral growth in cell culture, but negatively affected antigen stability [30]. H3N2 viruses grown in embryonated chicken eggs trigger conformational changes in the HA molecule under less acidic conditions than their antigenically similar primary isolates, and this phenotype was associated with the presence of amino acid substitutions A138S, L194P in HA1 and D160N in HA2, reduced resistance to acidic conditions and elevated temperatures [30]. Probably, the difference in pH levels during propagation in chicken embryos and cell culture caused the appearance of mutations in the region of the fusion peptide in HA2 in MDCK-adapted variants of the H3N2 vaccine strains Тех17-8, Тех17-16, Тех17-17 and H1N1 Calif17-8. Interestingly, that 5 mutations in the HA molecule were found only in the HA1 molecule, in particular, 4 of them (A138S, G218R, P221L and V223I) are located near the receptor-binding site [31]. The N165K mutation was localized in the HA antigenic site [31]. The A138S substitution can occur in vivo in immunocompromised patients as well as in vitro in MDCK cell culture and was found to cause a complete loss of α2,3-type receptor binding [32]. A mutation at position 218 in the HA1 molecule, which is located near the receptor-binding site, was also associated with decreased affinity for the human receptor and increased pathogenicity in a mouse model [33, 34]. The L194P amino acid substitution in HA1, which is prevalent in egg-adapted (passaged in embryonated chicken eggs 4–5 times) variants of H3N2 viruses, reduces binding and neutralization by broad-spectrum antibodies recognizing the receptor-binding site by 3 orders of magnitude, and also significantly changes the antigenicity of the HA molecule [35]. Despite the fact that some of the adaptation mutations detected in our study are located in significant places of the HA molecule, such as the receptor-binding site or antigenic sites, the described mutations do not affect the key parameters for the LAIV vaccine strain — the antigenicity of the MDCK-adapted strain and its immunogenicity do not change, but the replicative activity of the vaccine virus in cell culture increases, i.e., a useful property is acquired in the context of the production of cell-based LAIV. In this case, a decrease in infectious titers of MDCK-adapted LAIV strains in developing chicken embryos can be observed, which is an acceptable phenomenon when changing the substrate for culturing viruses. For the production of cultural LAIV, high replication activity in MDCK cell culture is most important, but not in eggs.
The influenza strain A/California/7/2009 (H1N1pdm) is genetically very similar to the A/California/4/2009 (H1N1pdm), but was isolated in the eggs and acquired the Q226R adaptation mutation during passaging, and after adaptation to mice, the N159D and K212M mutations were added. In this case, the virus with the Q226R mutation in HA1 lost affinity for human-type receptors and acquired affinity for avian receptors [36]. In both viruses, mutations located directly in the receptor-binding site expectedly affected the receptor specificity of the virus, disrupting the HA–NA balance, which led to a decrease in the reproductive activity of the virus in the MDCK-SIAT-1 cell culture. The mutations in the HA molecule that appeared after several more passages in mice became compensatory for the surface charge of the molecule and at the same time made a significant contribution to the increased pathogenicity of the studied viruses. Interestingly, data on the contribution of the D225E and Q226R mutations in HA to the virulence of the pandemic H1N1 influenza virus in mice were also obtained by Korean scientists [37]. In other studies, the N159D mutation is associated with escape mutations that allow the virus to evade the immune response [38].
During the preparation of the X-181 H1N1pdm09 vaccine strain in chicken embryos, the N133D, K212T and Q226R mutations were found in the HA1 molecule, which led to a strong change in the cross-reactivity of the vaccine strain, as a result of which the antibodies induced by the vaccine strain bound to the wild type of the virus, but did not neutralize it [39]. Evolutionary studies of the H1 molecule have shown the importance of amino acids at positions 156, 190 and 225 for adaptation to human receptors and antigenic drift of circulating H1N1 viruses [40].
Comparison of the H1N1pdm strains A/California/9/2007 and A/Brisbane/10/2010 revealed the presence of the E47K mutation in the HA2 molecule, which affected the stability of the HA trimer and decreased the threshold pH of membrane fusion from 5.4 to 5.0. It was also established that this occurs due to the presence of an intermonomer salt bridge between the amino acids K47 in HA2 and E21 in HA1 [41]. Furthermore, the E47K substitution increased the thermal stability of the virus and its virulence in ferrets, which indicates an advantage of the virus with K47 in HA2 in adapting to evolutionary changes in humans [42]. The V66H mutation in HA2 at the site of contact between two subunits of the HA molecule of the influenza A/WSN/33 (H1N1) virus affects the shift of the maximum pH of membrane fusion towards lower values (from 5.6 to 5.1). In this case, the ability of the virus to replicate in MDCK was reduced, which was accompanied by a longer clearance of the virus in mice [43]. It can be noted that the adaptation mutations A44V in Calif17-8 and K116E in Bolivia17-M, detected in the present study, have a similar localization with the already described mutations K47 in HA2 and E21 in HA1. Probably, they can affect the threshold pH value during membrane fusion, which is the expected result of virus adaptation to a new substrate. Based on the data obtained, the adaptation of the influenza A(H3N2) vaccine virus to the MDCK cell culture led to the emergence of multiple amino acid substitutions in HA. It was shown that the N154K and Y85E mutations, detected in the HA2 subunit of the HA molecule of the vaccine strain, are critical for virus replication in culture. Furthermore, the W92G, D160H adaptation mutations in HA2 provide a significant advantage for the replication of the vaccine virus in the MDCK cells over its replication in the embryonated chicken eggs.
Comparison of the steric arrangement of adaptation mutations between strains adapted to MDCK cells in laboratory and industrial conditions revealed the similarity of these positions. Thus, in the H1N1 strain, amino acid substitutions A44V (Calif17-4) and K116E (Bolivia17) are in close proximity to each other in the HA2 subunit of the HA stalk-domain, and most of the adaptation substitutions found in H3N2 strains are in the globular domain of the HA1 molecule (Fig. 6). Thus, adaptation of LAIV vaccine strains to MDCK cells in laboratory and industrial conditions leads to the appearance of similar adaptation substitutions in strains of the same subtype, with influenza B viruses being maximally stable, and A/H1N1 viruses acquiring adaptation substitutions necessary for enhanced virus replication in this substrate. Strains A/H3N2 are the least stable, and adaptation mutations can also affect receptor-binding regions, which indicates the need for careful monitoring of the antigenic properties of strains of this subtype during their production on a cell substrate.
Conclusion
As a result of adaptation of the A/17/California/2009/38 (H1N1pdm09) vaccine strain to the MDCK cells, mutations N156D in HA1 and A44V in HA2 were found. A study of their effect on replicative activity in vitro showed that the presence of both mutations increases the titer of the vaccine strain in the MDCK cell culture by an order of magnitude, which gives advantages to this variant when it is produced on an industrial scale. The detected mutations retained the immunogenicity, cross-reactivity and protective efficacy of the MDCK-adapted strain Calif17-8 at the level of the egg-derived vaccine strain Calif17. Thus, the conducted studies show that the vaccine strain of LAIV subtype H1N1pdm09, obtained by the method of classical reassortment in developing chicken embryos, can be used for the production of LAIV on the MDCK cells.
About the authors
Victoria A. Matyushenko
Institute of Experimental Medicine
Author for correspondence.
Email: matyshenko@iemspb.ru
ORCID iD: 0000-0002-4698-6085
researcher, Laboratory of immunology and vaccine prevention of viral infections, Department of virology named after A.A. Smorodintsev
Russian Federation, St. PetersburgArina D. Kostromitina
Institute of Experimental Medicine
Email: arina8goshina@gmail.com
ORCID iD: 0000-0001-5432-0171
junior researcher, Laboratory of cellular immunology, Department of immunology
Russian Federation, St. PetersburgEkaterina A. Stepanova
Institute of Experimental Medicine
Email: fedorova.iem@gmail.com
ORCID iD: 0000-0002-8670-8645
Cand. Sci. (Biol.), leading researcher, Department of virology named after A.A. Smorodintsev
Russian Federation, St. PetersburgLarisa G. Rudenko
Institute of Experimental Medicine
Email: vaccine@mail.ru
ORCID iD: 0000-0002-0107-9959
Dr. Sci. (Med.), Professor, main researcher, Laboratory of immunology and vaccine prevention of viral infections, Head, Department of virology named after A.A. Smorodintsev
Russian Federation, St. PetersburgIrina N. Isakova-Sivak
Institute of Experimental Medicine
Email: isakova.sivak@iemspb.ru
ORCID iD: 0000-0002-2801-1508
Dr. Sci. (Biol.), Corresponding Member of the Russian Academy of Sciences, Deputy director for science
Russian Federation, St. PetersburgReferences
- Tian Y., Ma Y., Ran J., et al. Protective impact of influenza vaccination on healthcare workers. Vaccines (Basel). 2024;12(11):1237. DOI: https://doi.org/10.3390/vaccines12111237
- Bouvier N.M. The future of influenza vaccines: a historical and clinical perspective. Vaccines (Basel). 2018;6(3):58. DOI: https://doi.org/10.3390/vaccines6030058
- Krietsch Boerner L. The flu shot and the egg. ACS Cent. Sci. 2020; 6(2):89–92. DOI: https://doi.org/10.1021/acscentsci.0c00107
- Charostad J., Rezaei Zadeh Rukerd M., Mahmoudvand S., et al. A comprehensive review of highly pathogenic avian influenza (HPAI) H5N1: An imminent threat at doorstep. Travel Med. Infect. Dis. 2023;55:102638. DOI: https://doi.org/10.1016/j.tmaid.2023.102638
- Rajaram S., Boikos C., Gelone D.K., Gandhi A. Influenza vaccines: the potential benefits of cell-culture isolation and manufacturing. Ther. Adv. Vaccines Immunother. 2020;8:2515135520908121. DOI: https://doi.org/10.1177/2515135520908121
- McGovern I., Taylor A., Sardesai A., et al. Influenza burden averted with a cell-based quadrivalent seasonal influenza vaccine compared with egg-based quadrivalent seasonal influenza vaccine. Expert Rev. Vaccines. 2024;23(1):371–9. DOI: https://doi.org/10.1080/14760584.2024.2330643
- Manini I., Domnich A., Amicizia D., et al. Flucelvax (Optaflu) for seasonal influenza. Expert Rev. Vaccines. 2015;14(6):789–804. DOI: https://doi.org/10.1586/14760584.2015.1039520
- Shcherbik S., Pearce N., Kiseleva I., et al. Implementation of new approaches for generating conventional reassortants for live attenuated influenza vaccine based on Russian master donor viruses. J. Virol. Methods. 2016;227:33–9. DOI: https://doi.org/10.1016/j.jviromet.2015.10.009
- Киселева И.В., Исакова И.Н., Ларионова Н.В. и др. Эффективность получения реассортантов между эпидемическими и холодоадаптированнымн вирусами гриппа в развивающихся куриныхэмбрионах и в культуре клеток MDCK. Журнал микробиологии, эпидемиологии и иммунобиологии. 2007;84(6):40–5. Kiseleva I.V., Isakova I.N., Larionova N.V., et al. Efficacy of production of reassortants between epidemic and cold-adapted influenza viruses in growing chicken embryos and in MDCK cell culture. Journal of Microbiology, Epidemiology and Immunobiology. 2007;84(6):40–5. EDN: https://elibrary.ru/iisqbx
- Rockman S., Laurie K., Ong C., et al. Cell-based manufacturing technology increases antigenic match of influenza vaccine and results in improved effectiveness. Vaccines (Basel). 2022;11(1):52. DOI: https://doi.org/10.3390/vaccines11010052
- Trager G., Kemble G., Schwartz R., et al. Methods of producing influenza vaccine compositions. Patent US No. 20060153872A1;2005.
- Нечаева Е.А., Сенькина Т.Ю., Радаева И.Ф. и др. Разработка технологии производства живой культуральной тривалентной вакцины против сезонного гриппа. Приоритетные направления развития науки и образования. 2016;(1):85–91. Nechaeva E.A., Sen'kina T.Yu., Radaeva I.F., et al. Development of technology for the production of a live culture trivalent vaccine against seasonal influenza. Priority Areas for the Development of Science and Education. 2016;(1):85–91. EDN: https://elibrary.ru/vkmwmr
- Ларионова Н.В., Киселева И.В., Руденко Л.Г., Александрова Г.И. Вакцинный штамм вируса гриппа А/17/Калифорния/2009/38 (H1N1) для производства живой гриппозной интраназальной вакцины для взрослых и для детей. Патент РФ № 2413765 C1;2011. Larionova N.V., Kiseleva I.V., Rudenko L.G., Aleksandrova G.I. Vaccine strain of influenza virus A/17/California/2009/38 (H1N1) for the production of live influenza intranasal vaccine for adults and children. Patent RF № 2413765 C1;2011.
- Дубровина И.А., Ларионова Н.В., Киселева И.В. и др. Штамм вируса гриппа А/17/Техас/2012/30 (H3N2) для производства живой гриппозной интраназальной вакцины для взрослых и для детей. Патент РФ № 2563352 C2;2015. Dubrovina I.A., Larionova N.V., Kiseleva I.V., et al. Influenza virus strain A/17/Texas/2012/30 (H3N2) for the production of live influenza intranasal vaccine for adults and children. Patent RF No. 2563352 C2;2015.
- Stepanova E., Krutikova E., Wong P.F., et al. Safety, immunogenicity, and protective efficacy of a chimeric A/B Live attenuated influenza vaccine in a mouse model. Microorganisms. 2021;9(2):259. DOI: https://doi.org/10.3390/microorganisms9020259
- Reed L.J., Muench H. A simple method of estimating fifty per cent endpoints. Am. J. Epidemiol. 1938;27(3):493–7.
- Isakova-Sivak I., Chen L.M., Matsuoka Y., et al. Genetic bases of the temperature-sensitive phenotype of a master donor virus used in live attenuated influenza vaccines: A/Leningrad/134/17/57 (H2N2). Virology. 2011;412(2):297–305. DOI: https://doi.org/10.1016/j.virol.2011.01.004 EDN: https://elibrary.ru/oiazrz
- Nechaeva E.A., Bogryantseva M.P., Ryzhikov A.B., et al. Phase I clinical trials of safety and immunogenicity of live cultural influenza vaccine vector-flu. BMC Proc. 2015;9(Suppl. 9):P73. DOI: https://doi.org/10.1186/1753-6561-9-S9-P73
- Pappas C., Viswanathan K., Chandrasekaran A., et al. Receptor specificity and transmission of H2N2 subtype viruses isolated from the pandemic of 1957. PloS One. 2010;5(6):e11158. https://doi.org/10.1371/journal.pone.0011158
- Thompson A.J., Wu N.C., Canales A., et al. Evolution of human H3N2 influenza virus receptor specificity has substantially expanded the receptor-binding domain site. Cell Host Microbe. 2024;32(2):261–75.e4. DOI: https://doi.org/10.1016/j.chom.2024.01.003
- Allen J.D., Ross T.M. H3N2 influenza viruses in humans: Viral mechanisms, evolution, and evaluation. Hum. Vaccin. Immunother. 2018;14(8):1840–7. DOI: https://doi.org/10.1080/21645515.2018.1462639
- Liu M., Bakker A.S., Narimatsu Y., et al. H3N2 influenza A virus gradually adapts to human-type receptor binding and entry specificity after the start of the 1968 pandemic. Proc. Natl Acad. Sci. USA. 2023;120(31):e2304992120. DOI: https://doi.org/10.1073/pnas.2304992120
- Martin E.T., Cheng C., Petrie J.G., et al. Low influenza vaccine effectiveness against A(H3N2)-associated hospitalizations in 2016–2017 and 2017–2018 of the Hospitalized Adult Influenza Vaccine Effectiveness Network (HAIVEN). J. Infect. Dis. 2021;223(12):2062–71. DOI: https://doi.org/10.1093/infdis/jiaa685
- Rondy M., Gherasim A., Casado I., et al. Low 2016/17 season vaccine effectiveness against hospitalised influenza A(H3N2) among elderly: awareness warranted for 2017/18 season. Euro Surveill. 2017;22(41):17-00645. DOI: https://doi.org/10.2807/1560-7917.es.2017.22.41.17-00645
- Kissling E., Pozo F., Buda S., et al. Low 2018/19 vaccine effectiveness against influenza A(H3N2) among 15-64-year-olds in Europe: exploration by birth cohort. Euro Surveill. 2019;24(48):1900604. DOI: https://doi.org/10.2807/1560-7917.es.2019.24.48.1900604
- Skowronski D.M., Sabaiduc S., Chambers C., et al. Mutations acquired during cell culture isolation may affect antigenic characterisation of influenza A(H3N2) clade 3C.2a viruses. Euro Surveill. 2016;21(3):30112. DOI: https://doi.org/10.2807/1560-7917.es.2016.21.3.30112
- Chambers B.S., Parkhouse K., Ross T.M., et al. Identification of Hemagglutinin Residues Responsible for H3N2 Antigenic Drift during the 2014-2015 Influenza Season. Cell Rep. 2015;12(1): 1–6. DOI: https://doi.org/10.1016/j.celrep.2015.06.005
- Lee H.K., Tang J.W., Kong D.H., et al. Comparison of mutation patterns in full-genome A/H3N2 influenza sequences obtained directly from clinical samples and the same samples after a single MDCK passage. PloS One. 2013;8(11):e79252. DOI: https://doi.org/10.1371/journal.pone.0079252
- Melidou A., Gioula G., Exindari M., et al. Ιnfluenza A(H3N2) genetic variants in vaccinated patients in northern Greece. J. Clin. Virol. 2017;94:29–32. DOI: https://doi.org/10.1016/j.jcv.2017.07.003
- Nakowitsch S., Waltenberger A.M., Wressnigg N., et al. Egg- or cell culture-derived hemagglutinin mutations impair virus stability and antigen content of inactivated influenza vaccines. Biotechnol. J. 2014;9(3):405–14. DOI: https://doi.org/10.1002/biot.201300225
- Skehel J.J., Wiley D.C. Receptor binding and membrane fusion in virus entry: the influenza hemagglutinin. Annu. Rev. Biochem. 2000;69:531–69. DOI: https://doi.org/10.1146/annurev.biochem.69.1.531
- Kumari K., Gulati S., Smith D.F., et al. Receptor binding specificity of recent human H3N2 influenza viruses. Virol. J. 2007;4:42. DOI: https://doi.org/10.1186/1743-422x-4-42
- Daniels P.S., Jeffries S., Yates P., et al. The receptor-binding and membrane-fusion properties of influenza virus variants selected using anti-haemagglutinin monoclonal antibodies. The EMBO J. 1987;6(5):1459–65. DOI: https://doi.org/10.1002/j.1460-2075.1987.tb02387.x
- Narasaraju T., Sim M.K., Ng H.H., et al. Adaptation of human influenza H3N2 virus in a mouse pneumonitis model: insights into viral virulence, tissue tropism and host pathogenesis. Microbes Infect. 2009;11(1):2–11. DOI: https://doi.org/10.1016/j.micinf.2008.09.013
- Wu N.C, Zost S.J., Thompson A.J., et al. A structural explanation for the low effectiveness of the seasonal influenza H3N2 vaccine. PLoS Pathog. 2017;13(10):e1006682. DOI: https://doi.org/10.1371/journal.ppat.1006682
- Гамбарян А.С., Ломакина Н.Ф., Боравлева Е.Ю. и др. Изменение вирулентности пандемического вируса гриппа A(H1N1), обусловленное мутациями гемагглютинина и полимеразы. Молекулярная биология. 2018;52(4):644–58. DOI: https://doi.org/10.1134/S0026898418040055 EDN: https://elibrary.ru/oxkwrn / Gambaryan A.S., Lomakina N.F., Boravleva E.Y., et al. Mutations in hemagglutinin and polymerase alter the virulence of pandemic A(H1N1) influenza virus. Molecular Biology. 2018;52(4):644–58. DOI: https://doi.org/10.1134/S0026893318040052 EDN: https://elibrary.ru/ybidnj
- Kim J.I., Lee I., Park S., et al. Effects of a hemagglutinin D222G substitution on the pathogenicity of 2009 influenza A (H1N1) virus in mice. Arch Virol. 2014;159(10):2559–65. DOI: https://doi.org/10.1007/s00705-014-2104-5
- Rudneva I., Ignatieva A., Timofeeva T., et al. Escape mutants of pandemic influenza A/H1N1 2009 virus: variations in antigenic specificity and receptor affinity of the hemagglutinin. Virus Res. 2012;166(1-2):61–7. DOI: https://doi.org/10.1016/j.virusres.2012.03.003
- Raymond D.D., Stewart S.M., Lee J., et al. Influenza immunization elicits antibodies specific for an egg-adapted vaccine strain. Nat. Med. 2016;22(12):1465–9. DOI: https://doi.org/10.1038/nm.4223
- Shen J., Ma J., Wang Q. Evolutionary trends of A(H1N1) influenza virus hemagglutinin since 1918. PloS One. 2009;4(11):e7789. DOI: https://doi.org/10.1371/journal.pone.0007789
- Cotter C.R., Jin H., Chen Z. A single amino acid in the stalk region of the H1N1pdm influenza virus HA protein affects viral fusion, stability and infectivity. PLoS Pathog. 2014;10(1):e1003831. DOI: https://doi.org/10.1371/journal.ppat.1003831
- Yang H., Chang J.C., Guo Z., et al. Structural stability of influenza A(H1N1)pdm09 virus hemagglutinins. J. Virol. 2014;88(9): 4828–38. DOI: https://doi.org/10.1128/jvi.02278-13
- Jakubcová L., Vozárová M., Hollý J., et al. Biological properties of influenza A virus mutants with amino acid substitutions in the HA2 glycoprotein of the HA1/HA2 interaction region. J. Gen. Virol. 2019;100(9):1282–92. DOI: https://doi.org/10.1099/jgv.0.001305
Supplementary files