Analysis of entomological indicators and distribution of Aedes aegypti larvae in dengue endemic areas
- Authors: Sutriyawan A.1, Manap A.2, Sulami N.3, Setiyadi A.4, Riskiah D.M.3, Kurniawati R.D.1, Khariri K.5
-
Affiliations:
- Bhakti Kencana University
- University of Jayabaya
- Midwifery Academy of Surya Mandiri Bima
- Binawan University
- National Research and Innovation Agency
- Issue: Vol 100, No 4 (2023)
- Pages: 314-320
- Section: ORIGINAL RESEARCHES
- URL: https://microbiol.crie.ru/jour/article/view/11274
- DOI: https://doi.org/10.36233/0372-9311-406
- EDN: https://elibrary.ru/rjjnhz
- ID: 11274
Cite item
Full Text
Abstract
Background. The cause of dengue fever’s endemicity is vector larvae density, with Aedes aegypti as the prime vector. Bandung municipality is a high dengue fever endemic area. Hence, studying the habitat characteristics of the Aedes mosquito is essential to controlling the populations of mosquitos.
Purpose. This study aimed to identify the aedes larvae breeding sites and the relationship between the breeding risk index, hygiene risk index, maya index, and the existence of larvae with the incidence of dengue fever.
Method. The design used in this research was a cross-sectional survey. The sampling technique used simple random sampling. The quantity of the sample was 544 directly observed houses.
Results. The entomological parameters obtained were house index (23.89%), container index (7.81%), Breteau index (50.73%), and larva free number (76.10%). The breeding risk index, hygiene risk index, and maya index are in the low category. The chi-square test conveyed that the breeding risk index, maya index, and the existence of larvae were significantly associated with the incidence of dengue fever.
Conclusion. The entomological index may influence the high incidence of dengue fever. These findings and results may help the authorities to improve mosquito nest eradication in attempts to prevent dengue transmission.
Full Text
Introduction
Dengue is still a global public health issue, particularly in tropical and subtropical areas, including Indonesia as one of the dengue endemic countries [1]. Dengue is a disease caused by the dengue virus which has the fastest spread worldwide [2]. The global incidence of dengue has risen significantly, with approximately half of the world's population at risk. Although an estimated 100–400 million infections occur yearly, more than 80% are generally milder and asymptomatic1.
Dengue is a disease which causes death due to bleeding and hemodynamic disorders. The primary vector of dengue is the Aedes aegypti mosquito, whereas the potential vector is Ae. albopictus. These mosquitoes are also vectors of chikungunya, yellow fever, and zika virus [3]. Specific medicines and vaccines that are efficacious for dengue are still under investigation, since no particular drug is efficacious in the treatment of dengue [4].
Indonesia is a dengue-endemic country. 248,127 cases were reported in 2019. Meanwhile, until July 2020, the number of cases had reached 71,633 cases2. An epidemiological study of dengue fever in Bandung Municipality stated that the existence of Ae. aegypti mosquito larvae highly influences the high number of infection cases [5]. Prevention and management of dengue fever depends on effective vector control measures. Sustained community involvement can substantially improve vector control efforts.
Multiple factors have been implicated in the global resurgence of dengue fever. These include failure to control aedes populations, uncontrolled urbanization, and unprecedented population growth [6]. The seasonal dynamics of Ae. aegypti population sizes generally have a positive relationship with climatic variables such as temperature, rainfall, and relative humidity [7]. Previous studies have indicated that the distribution pattern of dengue can be affected by various factors, one of which is the existence of mosquito vectors that can be assessed through entomological indexes such as: House Index (HI), Container Index (CI), Breteau Index (BI), and Mosquito larva Free Rate (ABJ). High dengue disease transmission is encouraged by the high density of Ae. aegypti mosquitoes [7, 8].
Current prevention efforts include Mosquito Nest Eradication (Pemberantasan Sarang Nyamuk, or PSN), but implementation still needs to be optimized. One of the efforts that have proven effective is to reduce and suppress the mosquito population. WHO states that effective dengue prevention is achievable by controlling vectors from larvae to adult mosquitoes [9]. In dengue eradication programs, the typical larval survey is the investigation of Ae. aegypti larvae in residential and communal areas using the single larva method [10].
With an increasing tendency of dengue incidence, especially in Bandung Municipalities, the research focus has been on case tracing and control of Ae. aegypti. Therefore, there is a need to conduct a study of distribution patterns based on entomological indicators. This program will be very useful when used as basic literature. It can also form the basis for making vector control policies more precisely targeted in an effort to prevent dengue fever. Vector population density can help programs determine the rate of speed of the dengue virus spread in a particular area [11]. This research aims to identify the breeding sites of Aedes larvae and the association of the Breeding risk index (BRI), Hygiene risk index (HRI), Maya index (MI), and the occurrence of larvae with the incidence of dengue fever. The findings of this research can serve as a foundation for dengue fever prevention efforts through effective mosquito nest eradication efforts.
Materials and methods
Research design
This research used a cross-sectional design. This study was conducted in Bandung City in March–July 2022. This study surveyed each endemic area. Each stratification selected nine sub-districts based on a purposive sampling design.
Sampling technique
The population in this research was heads of households from all residents of Bandung City. The sample selection of endemic sub-districts was based on sub-districts with the highest number of cases by considering existing incidence rate data and stratification based on the Bandung City health office in 2021. 544 houses were taken using the Sample Size for One Sample Test of Proportion formula (level of significance 5%, power 90%). The sample houses were chosen using a random sampling method from the combined list of residents owned by each sub-district. A house was sampled, if selected as a sample and willing to be visited.
Entomology survey
Surveys were conducted on larvae by examining all water storage containers accessible from respondents' homes, in order to determine the most effective and efficient types of containers for mosquito breeding. Surveys were conducted on wet containers filled with water at the time of the survey. Samples of larvae found were collected using a net (tea strainer) and then placed in small plastic jars filled with water. Each sample jar was labeled with the identification number, date, location, and number of larvae gathered. Breeding sites of the mosquito species collected were recorded in pre-determined survey data sheets during sample collection. Containers were recorded as positive for Aedes, if larvae were found in the water storage containers.
Containers classification
Containers were categorized into three groups based on their purpose: Controllable containers, disposable containers, and under-controllable containers. Water storage containers recorded in the survey as controlled containers are places that can be maintained or controlled, such as bathtubs, water tanks, buckets, jerry cans, wells, flowerpots, drums, refrigerators, dispensers, barrels, animal drinkers, crocks and gutters. Used containers are waste or places that are no longer used, such as used cans, tires, bottles, buckets, jars, glasses, and drums. Furthermore, containers such as fishponds and aquariums were deemed under-controllable.
Larvae identification
After being collected, the larvae were taken to the parasitology laboratory of Bhakti Kencana University. The larvae were identified under a microscope in the laboratory. Species identification was finalized using standard identification keys explained in the literature "Pictorial keys for identifying mosquitoes (Diptera: Culicidae) associated with Dengue Virus Transmission” [12]. Furthermore, laboratory results were then recorded on the appropriate survey sheet.
Data analysis
Maya index and entomological index analysis were used to illustrate the transmission risk of dengue. Dominant containers were identified by data collection on the containers with the highest number of positive larvae found inside and outside the house. Containers in this regard were grouped into two categories: controlled containers and used containers. The Maya Index in this research was determined using two indicators: BRI and HRI. BRI is each house's proportion of controllable sites. BRI is obtained by dividing the number of controllable areas examined by the average number of containers in the house. The HRI is each house's proportion of disposable sites. HRI is calculated by dividing the number of disposable sites in the examined homes by the average number of containers in the home [13]. BRI, HRI, and MI values were classified into three categories: high, medium, and low, based on Lozano's distribution (2002). MI is determined from the BRI and HRI values in each house arranged in a 3 × 3 matrix [14].
Entomological indicators, namely HI, CI, and BI, are categorized based on the larval density index according to the density figure (DF) value in the low, medium, and high categories [17]. CI is an index used to define the number of larvae-positive containers out of all containers examined (Number of larvae-positive containers × 100% / Number of containers discussed). HI is an index used to identify the number of larvae-positive houses out of all homes inspected (Number of larvae-positive homes × 100% / Number of homes inspected). BI is an index used to determine how many larvae-positive containers out of all the homes examined (Number of larvae-positive containers × 100% / Number of homes examined). The entomological index defines the risk of infection based on DF. The low density is categorized as DF 1, medium density as DF 2–5, and high density as DF 6–9 [11]. The determination of the density of index larvae based on HI, CI, and BI taken from the MW Service can be seen in Table 1. MI analysis is determined by identifying controlled and uncontrolled water reservoirs, namely the categories of controllable sites and disposable sites.
Table 1. Density of Aedes Aegypti Larvae Based on DF and Indicators of HI, CI, and BI
DF | HI | CI | BI |
1 | 1–3 | 1–2 | 1–4 |
2 | 4–7 | 3–5 | 5–9 |
3 | 8–17 | 6–9 | 10–19 |
4 | 18–29 | 10–14 | 20–34 |
5 | 30–37 | 15–20 | 35–49 |
6 | 38–49 | 21–27 | 50–74 |
7 | 50–59 | 28–31 | 75–99 |
8 | 60–76 | 32–40 | 100–199 |
9 | – | – | – |
Source: Service, MW. Mosquito Ecology Field Sampling Methods. Chapman and Hal.
The Chi-Square test was used for further analysis. This test was used to analyze the relationship between the Maya index and the occurrence of larvae with the dengue incidence, with a significance level of 5%.
Results
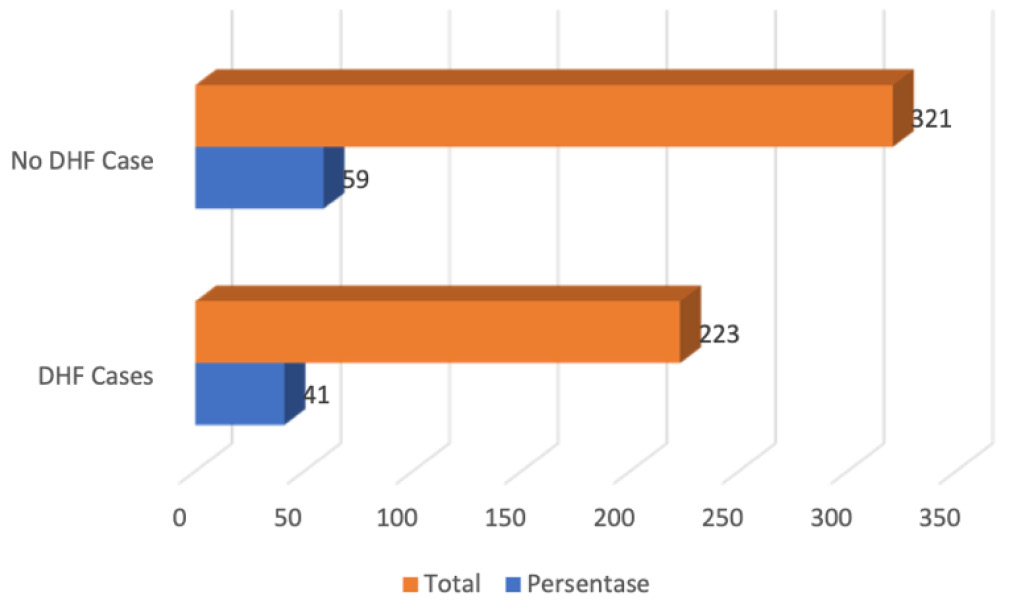
This study was conducted on 544 homes and resulted in an incidence rate of 41% (Fig. 1). The elevation of dengue incidence is relevant to the number of larvae found in the houses. A total of 276 containers containing larvae were found. The majority of mosquito larvae were found in bathtubs (52), dispensers (40), refrigerators (30), buckets (24), bottles (23), and used tires (13). At the same time, wells, barrels, crocks, used jars, used cups, used drums, fishponds, and aquariums were not found with any larvae at all. Most mosquito larvae were found in controllable containers (Fig. 2).
Fig. 1. Prevalence of dengue in Bandung municipality.
Fig. 2. Containers varieties on households in Bbandung municipality.
The MI status is based on potential mosquito breeding sites (BRI) and environmental cleanness (HRI). MI analysis (Table 2) conveys that BRI, HRI, and MI values di Kota Bandung are primarily in the low category.
Table 2. The proportion of households based on the Breeding Risk Index (BRI), Hygiene Risk Index (HRI), and Maya Index (MI) in Bandung municipality
Category | BRI | HRI | MI | |||
n | % | n | % | n | % | |
Low | 428 | 78.7 | 491 | 90.3 | 420 | 77.2 |
Medium | 7 | 1.3 | 7 | 1.3 | 83 | 15.3 |
High | 109 | 20 | 46 | 8.5 | 41 | 7.5 |
Total | 544 | 100 | 544 | 100 | 544 | 100 |
Entomological indicators in the form of index measurement of Aedes aegypti larval density in particular settlements are essential considerations in effective vector control. Table 3 shows that the HI was 23.89%, the CI was 7.81%, the BI was 50.73%, and ABJ was 76.10%.
Table 3. Entomological Index
Entomological Index | Result, % | DF |
House Index | 23,89 | 4 |
Container Index | 7,81 | 3 |
Breteau Index | 50,73 | 6 |
Larvae Free Number | 76,10 |
The effect of the Entomology Index on dengue incidence in Bandung Municipality can be seen in Table 4. BRI is a factor that affects the elevation in dengue cases (p = 0,001). MI is a factor that influences the peak of dengue cases (p = 0,001). The presence of larvae is also a factor that causes an increase in dengue cases in Bandung municipality (p = 0,000). Meanwhile, the writer concludes that HRI could not be proven to influence the increase in dengue cases.
Table 4. The effect of Entomological Index on the incidence of dengue
Entomological Index | No Dengue | Dengue | Total | p-value | |||
n | % | n | % | n | % | ||
Breeding Risk Index (BRI) | 0,001 | ||||||
low | 235 | 54,9 | 193 | 45,1 | 428 | 100 | |
medium | 6 | 85,7 | 1 | 14,3 | 7 | 100 | |
high | 80 | 73,4 | 29 | 26,6 | 109 | 100 | |
Hygine Risk index (HRI) | 0,378 | ||||||
low | 285 | 58,0 | 206 | 42,0 | 491 | 100 | |
medium | 5 | 71,4 | 2 | 28,6 | 7 | 100 | |
high | 31 | 67,4 | 15 | 32,6 | 46 | 100 | |
Maya Index (MI) | 0,001 | ||||||
low | 231 | 55,0 | 189 | 45,0 | 420 | 100 | |
medium | 63 | 75,9 | 20 | 24,1 | 83 | 100 | |
high | 27 | 65,9 | 14 | 34,1 | 41 | 100 | |
Presence of Larvae | 0,000 | ||||||
absent | 224 | 54,1 | 190 | 45,9 | 414 | 100 | |
present | 97 | 74,6 | 33 | 25,3 | 130 | 100 | |
Discussion
Common breeding sites observed in the study area were bathtubs, dispensers, refrigerators, barrels, and used plastic. Most residents in Bandung municipality store tap water and rainwater in containers for household necessities. Based on the research results, the incidence of dengue in Bandung City is quite inflated. This result is relevant to the data of dengue in Indonesia. Over a 50-year period, there has been a sharp increase in the annual IR of dengue in Indonesia, from only 0.05 cases per 100,000 person-years in 1968 to 77.96 cases per 100,000 person-years in 2016 [2]. The elevation of dengue cases in Bandung Municipality is reciprocal to the high number of mosquito larvae found. Thus, the writer examined different containers in respondents' homes in Bandung Municipality and identified Aedes aegypti larvae and pupae. These findings are consistent with previous studies or research [16, 17]. A significant number of Aedes aegypti larvae were found, since the study site was in an urban area. Findings in Southern Taiwan show that Aedes aegypti almost exclusively exists in urban areas [18]. While the conclusions from a study in East Ethiopia from 405 containers were positive for mosquito larvae, 84.4% were identified as Aedes aegypti [19].
Nevertheless, in our research, Aedes aegypti was found to be the most dominant species to breed in artificial containers. Many containers are located near human habitation and are potentially more durable than natural containers [20]. In our research, no Anopheles mosquito larvae were found. Nonetheless, Anopheles mosquitoes inhabit old tires in Nicholas County, West Virginia [21]. The type of container, water quality, and condition of the water container are important for breeding3.
HI, CI, BI, and ABJ were relatively low. These findings are consistent and in line with the study that sta-
ted an overall HI of 14.2%, BI of 24.65, and CI of 5.9%
[22]. All indices indicate a high level of risk of dengue transmission. A survey in Nepal found CI to be higher in the transitional period than in the rainy season [17]. A recent study in Malaysia conveyed maximum HI = 13,33%, BI = 13, dan CI = 19,05% [23]. In the literature, it has been criticized that this index needs more operational value and usage in assessing transmission risk. However, this index indicates a threat of global transmission at the community level [17]. The majority of Aedes aegypti larvae were found inside the respondents' homes. In accordance with findings in Southern Mexico, the frequency of larval populations was higher inside the households (14.1%) compared to containers found outdoors (5.1%) [24]. The writers found the most Aedes aegypti larvae in bathtubs, comparably with findings in Thailand that stated the most important risk factors for the existence of Aedes aegypti were container type (jars and tanks), location (toilet/bathroom), and lid status (no lid or covering) [25].
Amongst the risk factors for dengue incidence is the MI. In order to obtain the MI, the BRI and HRI were first calculated using the Miller formula [26]. The writers found that MI was in a low category. Another study in Tegal City stated that there was no difference between low and medium index MI categories. Thus, houses with low and medium index status have the equivalent risk of dengue infection [27]. The writers found that the most frequently controlled containers were bathtubs, buckets, jerry cans, refrigerators, dispensers, animal drinkers, and drums. Research in Semarang conveyed that mosquito larvae were primarily found in flowerpots and buckets, while those who suffered from dengue found the most mosquito larvae in bathtubs [28].
In this finding, BRI is in a low category, meaning that the danger as a mosquito breeding site is insufficient. This is consistent with other findings stating that the city is at low risk of mosquito breeding [29, 30]. Another research in Central Java found that BRI was at medium risk [31]. Several larvae were found in controlled containers, and all of them were Aedes aegypti larvae. The study in Eastern Ethiopia stated that the mosquito larvae-positive containers were mostly artificial water storage containers located outdoors (93.06%), open or partially covered (87.6%), and fully or partially exposed to sunlight (67.86%) [19].
The existence of mosquito larvae in the home can elevate the risk of dengue transmission. If there are mosquito larvae around the house, either indoors or outdoors, it will increase the risk of dengue infection. A study in Japan indicated that the highest number of wet containers were outdoors (56.5%), followed by indoors (32.2%) and roofs (11.3%). Among outdoor containers, 7.8% of containers were found to be overrun with Aedes larvae. Among indoor and rooftop containers, 3.1% and 3.9% of containers were found positive, respectively. The overall HI was 14.2. BI was 24.6, and the CI was 5.9 [23]. All indexes showed that the transmission risk rate is currently high [32, 33]. So it is necessary to elevate efforts to prevent dengue by implementing mosquito nest eradication.
Conclusion
The study detected larval density based on entomological indices in the medium and high categories. BRI, MI, and larval occurrence can significantly elevate the incidence of dengue fever in Bandung Municipality. The writers suggest dengue vector control through routine inspection and destruction of potential container types both inside and outside the house as a preventive measure for dengue fever transmission.
Funding source. This study was not supported by any external sources of funding.
Conflict of interest. The authors declare no apparent or potential conflicts of interest related to the publication of this article.
Author contribution. Аll authors made a substantial contribution to the conception of the work, acquisition, analysis, interpretation of data for the work, drafting and revising the work, final approval of the version to be published.
1 WHO. Dengue and severe dengue; 2023. URL: https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue
2 Kementrian Kesehatan Republik Indonesia. Kemenkes R.I. Profil Kesehatan Indonesia 2020. Jakarta;2021. URL: https://www.kemkes.go.id/downloads/resources/download/pusdatin/profil-kesehatan-indonesia/Profil-Kesehatan-Indonesia-Tahun-2020.pdf
3 WHO. Chen C.D., Lee H.L., Stella-Wong S.P., et al. Container survey of mosquito breeding sites in a university campus in Kuala Lumpur, Malaysia; 2009. URL: https://apps.who.int/iris/handle/10665/170721
About the authors
Agung Sutriyawan
Bhakti Kencana University
Author for correspondence.
Email: agung.sutriawan@bku.ac.id
ORCID iD: 0000-0002-6119-6073
Researcher, Head, Department of Public Health, Faculty of Health Sciences
Indonesia, BandungAbdul Manap
University of Jayabaya
Email: hamanap.joyo@gmail.com
ORCID iD: 0009-0005-1788-4118
Senior Researcher, Department of Management, Faculty of Economics and Business
Indonesia, JakartaNeti Sulami
Midwifery Academy of Surya Mandiri Bima
Email: neti.sulami@gmail.com
ORCID iD: 0000-0003-3446-3153
Researcher, Department of Midwifery
Indonesia, BimaAgung Setiyadi
Binawan University
Email: agung.setiyadi@binawan.ac.id
ORCID iD: 0000-0001-8338-1803
Researcher, Department of Nursing, Faculty of Nursing and Midwifery
Indonesia, JakartaDian Mariza Riskiah
Midwifery Academy of Surya Mandiri Bima
Email: dianurindo@gmail.com
ORCID iD: 0009-0006-4192-595X
Researcher, Department of Midwifery
Indonesia, BimaRatna Dian Kurniawati
Bhakti Kencana University
Email: ratna.dian@bku.ac.id
ORCID iD: 0000-0002-7042-3696
Senior Researcher, Dean, Faculty of Health Sciences
Indonesia, BandungKhariri Khariri
National Research and Innovation Agency
Email: arie.tegale@gmail.com
ORCID iD: 0000-0003-2794-774X
Researcher, Faculty of Medicine, Member of National Research and Innovation Agency
Indonesia, JakartaReferences
- Lesmana S.D., Maryanti E., Susanty E., et al. Organophosphate resistance in Aedes aegypti: study from dengue hemorrhagic fever endemic subdistrict in Riau, Indonesia. Rep. Biochem. Mol. Biol. 2022;10(4):589–96. DOI: https://doi.org/10.52547/rbmb.10.4.589
- Harapan H., Michie A., Mudatsir M., et al. Epidemiology of dengue hemorrhagic fever in Indonesia: analysis of five decades data from the National Disease Surveillance. BMC Res. Notes. 2019;12(1):350. DOI: https://doi.org/10.1186/s13104-019-4379-9
- Kraemer M.U.G., Sinka M.E., Duda K.A., et al. The global distribution of the arbovirus vectors Aedes aegypti and Ae. albopictus. eLife. 2015;4:e08347. DOI: https://doi.org/10.7554/eLife.08347
- Deng S.Q., Yang X., Wei Y., et al. A review on dengue vaccine development. Vaccines (Basel). 2020;8(1):63. DOI: https://doi.org/10.3390/vaccines8010063
- Sutriyawan A., Herdianti H., Cakranegara P.A., et al. Predictive index using receiver operating characteristic and trend analysis of dengue hemorrhagic fever incidence. Open Access Maced. J. Med. Sci. 2022;10(E):681–7. DOI: https://doi.org/10.3889/oamjms.2022.8975
- Kampango A., Furu P., Sarath D.L., et al. Risk factors for occurrence and abundance of Aedes aegypti and Aedes bromeliae at hotel compounds in Zanzibar. Parasit. Vectors. 2021;14(1):544. DOI: https://doi.org/10.1186/s13071-021-05005-9
- Rahayu A., Saraswati U., Supriyati E., et al. Prevalence and distribution of dengue virus in Aedes aegypti in Yogyakarta city before deployment of Wolbachia infected Aedes aegypti. Int. J. Environ. Res. Public Health. 2019;16(10):1742. DOI: https://doi.org/10.3390/ijerph16101742
- Handayani M.T., Raharjo M., Joko T. Pengaruh Indeks Entomologi dan Sebaran Kasus Demam Berdarah Dengue di Kabupaten Sukoharjo. J. kesehat. lingkung. Indones. 2023;22(1):46–54. DOI: https://doi.org/10.14710/jkli.22.1.46-54
- Fuadzy H., Hendri J. Indeks entomologi dan kerentanan larva Aedes aegypti terhadap temefos di Kelurahan Karsamenak Kecamatan Kawalu Kota Tasikmalaya. Vektora: Jurnal Vektor dan Reservoir Penyakit. 2015;7(2):57–64.
- Prasetyowati H. Gambaran Maya Indeks dan Kepadatan Larva di Daerah Endemis Dbd Jakarta Timur. Vektora: Jurnal Vektor dan Reservoir Penyakit. 2017;9(1):43–9.
- Hartati R., Satoto T.B.T., Murhandarwati E.H., Widawati M. Analisis Indikator Entomologi dan Sebaran Jentik Aedes aegypti pada Daerah Stratifi kasi Endemisitas Demam Berdarah Dengue di Kota Jayapura. ASPIRATOR J. Vector Borne Dis. Stud. 2021;13(2):127–36. DOI: https://doi.org/10.22435/asp.v13i2.4441
- Rueda L.M. Pictorial keys for the identification of mosquitoes (Diptera: Culicidae) associated with Dengue Virus Transmission. Zootaxa. 2004;589(1). DOI: https://doi.org/10.11646/zootaxa.589.1.1
- Halstead S.B. Community-based dengue control: a description and critique of the Rockefeller Foundation Program. Trop. Med. 1994;35(4):285–91.
- Danis-Lozano R., Rodríguez M.H., Hernández-Avila M. Gender-related family head schooling and Aedes aegypti larval breeding risk in Southern Mexico. Salud Publica Mex. 2002;44(3):237–42. DOI: https://doi.org/10.1590/s0036-36342002000300007
- Guzman M.G., Harris E. Dengue. Lancet. 2015;385(9966): 453–65. DOI: https://doi.org/10.1016/S0140-6736(14)60572-9
- Dhar-Chowdhury P., Haque C.E., Lindsay R., Hossain S. Socioeconomic and ecological factors influencing Aedes aegypti prevalence, abundance, and distribution in Dhaka, Bangladesh. Am. J. Trop. Med. Hyg. 2016;94(6):1223–33. DOI: https://doi.org/10.4269/ajtmh.15-0639
- Rahman M., Faruk M., Tanjila S., et al. Entomological survey for identification of Aedes larval breeding sites and their distribution in Chattogram, Bangladesh. Beni Suef Univ. J. Basic Appl. Sci. 2021;10(1):1–11. DOI: https://doi.org/10.1186/s43088-021-00122-x
- Lin C.H., Schiøler K.L., Ekstrøm C.T., et al. Location, seasonal, and functional characteristics of water holding containers with juvenile and pupal Aedes aegypti in Southern Taiwan: A cross-sectional study using hurdle model analyses. PLoS Negl. Trop. Dis. 2018;12(10):e0006882. DOI: https://doi.org/10.1371/journal.pntd.0006882
- Getachew D., Tekie H., Gebre-Michael T., et al. Breeding sites of Aedes aegypti: potential dengue vectors in Dire Dawa, East Ethiopia. Interdiscip. Perspect. Infect. Dis. 2015;2015:706276. DOI: https://doi.org/10.1155/2015/706276
- Yee D.A., Kneitel J.M., Juliano S.A. Environmental correlates of abundances of mosquito species and stages in discarded vehicle tires. J. Med. Entomol. 2010;47(1):53–62. DOI: https://doi.org/10.1093/jmedent/47.1.53
- Joy J.E., Hanna A.A., Kennedy B.A. Spatial and temporal variation in the mosquitoes (Diptera: Culicidae) inhabiting waste tires in Nicholas County, West Virginia. J. Med. Entomol. 2003; 40(1):73–7. DOI: https://doi.org/10.1603/0022-2585-40.1.73
- Ferdousi F., Yoshimatsu S., Ma E., et al. Identification of essential containers for Aedes larval breeding to control dengue in Dhaka, Bangladesh. Trop. Med. Health. 2015;43(4):253–64. DOI: https://doi.org/10.2149/tmh.2015-16
- Mahmud M.A.F., Mutalip M.H., Lodz N.A., Shahar H. Study on key Aedes spp breeding containers in dengue outbreak localities in Cheras district, Kuala Lumpur. Int. J. Mosq. Res. 2018;5(2):23–30.
- Valdez-Delgado K.M., Moo-Llanes D.A., Danis-Lozano R., et al. Field effectiveness of drones to identify potential Aedes aegypti breeding sites in household environments from Tapachula, a dengue-endemic city in southern Mexico. Insects. 2021;12(8):663. DOI: https://doi.org/10.3390/insects12080663
- Vannavong N., Seidu R., Stenström T.A., et al. Effects of socio-demographic characteristics and household water management on Aedes aegypti production in suburban and rural villages in Laos and Thailand. Parasit. Vectors. 2017;10(1):170. DOI: https://doi.org/10.1186/s13071-017-2107-7
- Miller J.E., Martínez-Balanzar A., Gazga-Salinas D. Where Aedes aegypti live in Guerrero; using the Maya index to measure breeding risk. In: Dengue: A Worldwide Problem, a Common Strategy. México;1992:311–7.
- Rokhmawanti N., Ginanadjar P., Martini M. Hubungan Maya Index dengan Kejadian Demam Berdarah Dengue di Kelurahan Tegalsari Kota Tegal. Jurnal Kesehatan Masyarakat Universitas Diponegoro. 2015;3(1):162–70. DOI: https://doi.org/10.14710/jkm.v3i1.11339
- Dewi A.A.K., Sukendra D.M. Maya Index dan Karakteristik Lingkungan Area Rumah dengan Kejadian Demam Berdarah Dengue. HIGEIA J. Publ. Health Res. Dev. 2018;2(4):531–42. DOI: https://doi.org/10.15294/higeia.v2i4.24699
- Udayanga L., Gunathilaka N., Iqbal M.C.M., et al. Empirical optimization of risk thresholds for dengue: an approach towards entomological management of Aedes mosquitoes based on larval indices in the Kandy District of Sri Lanka. Parasit. Vectors. 2018;11(1):368. DOI: https://doi.org/10.1186/s13071-018-2961-y
- Muñiz-Sánchez V., Valdez-Delgado K.M., Hernandez-Lopez F.J., et al. Use of unmanned aerial vehicles for building a house risk index of mosquito-borne viral diseases. Machines. 2022;10(12):1161. DOI: https://doi.org/10.3390/machines10121161
- Pascawati N.A., Songjanan E.P., Satoto T.B.T., Deta E. Improvement to early warning system of DHF transmission through controlling vector breeding places of Aedes sp. in Klaten District, Central Java. J. Publ. Health Trop. Coast. Reg. 2018;1(1):20–6. DOI: https://doi.org/10.14710/jphtcr.v1i1.3245
- Mboera L.E.G., Mweya C.N., Rumisha S.F., et al. The risk of dengue virus transmission in Dar es Salaam, Tanzania during an epidemic period of 2014. PLoS Negl. Trop. Dis. 2016;10(1):e0004313. DOI: https://doi.org/10.1371/journal.pntd.0004313
- Barbosa G.L., Donalísio M.R., Stephan C., et al. Spatial distribution of the risk of dengue and the entomological indicators in Sumaré, State of São Paulo, Brazil. PLoS Negl. Trop Dis. 2014;8(5):e2873. DOI: https://doi.org/10.1371/journal.pntd.0002873