Biological characterization of cold-adapted SARS-CoV-2 variants
- Authors: Faizuloev E.B.1, Korchevaya E.R.1, Gracheva A.V.1, Samoilikov R.V.1, Smirnova D.I.1, Sokolova O.S.2, Glukhov G.S.2, Moiseenko A.V.2, Leneva I.A.1, Nagieva F.G.1, Svitich O.A.1,3, Zverev V.V.1,3
-
Affiliations:
- I.I. Mechnikov Research Institute of Vaccines and Sera
- Lomonosov Moscow State University, Faculty of Biology
- I.M. Sechenov First Moscow State Medical University (Sechenov University)
- Issue: Vol 99, No 4 (2022)
- Pages: 397-409
- Section: ORIGINAL RESEARCHES
- URL: https://microbiol.crie.ru/jour/article/view/1304
- DOI: https://doi.org/10.36233/0372-9311-280
- ID: 1304
Cite item
Abstract
Introduction. The emergence of new epidemiologically significant variants of SARS-CoV-2 has shifted emphasis to development of a live vaccine, which would be able to provide protection against a wide range of antigenic variants of the virus.
The aim of the study was to obtain SARS-CoV-2 variants attenuated through cold adaptation and to provide their biological characterization.
Materials and methods. The Dubrovka laboratory strain of SARS-CoV-2 and its variants were cultured on Vero and Calu-3 cells. The virus quantification was performed by virus titration in Vero cells and by real-time reverse transcription-polymerase chain reaction. SARS-CoV-2 virions were analyzed using transmission electron microscopy. Genome sequences of the virus were identified by nanopore sequencing. The attenuation (att) phenotype of SARS-CoV-2 variants was identified using Syrian hamsters as an animal model for COVID-19.
Results. Cold-adapted (ca) SARS-CoV-2 variants – Dubrovka-ca-B4 and Dubrovka-ca-D2 were produced by continued passaging of the Dubrovka strain in the Vero cell culture at the temperature being gradually decreased to 23ºC and by subsequent cloning. Up to 20 nucleotide substitutions and 18 amino acid substitutions were detected in genomes of ca-variants. Ca-variants, as distinct from the parent Dubrovka strain, actively replicated at 23ºC, while the Dubrovka-ca-D2 variant had a temperature-sensitive (ts) phenotype (did not replicate at 39ºC). Ca-variants of the virus replicated poorly at 37ºC in the Calu-3 human lung cell culture, which, along with the ts-phenotype, can be a marker of virus attenuation for humans. In the intranasally infected Syrian hamsters, ca-variants of the virus demonstrated an attenuation phenotype: they did not cause loss of appetite, fatigue, drowsiness, did not slow down weight gain, replicating much more slowly in the lungs and brain compared to the virulent Dubrovka strain.
Conclusion. The obtained attenuated SARS-CoV-2 ca-variants, Dubrovka-ca-B4 and Dubrovka-ca-D2, should be studied further as candidate vaccine strains for a live attenuated vaccine against COVID-19.
Keywords
Full Text
INTRODUCTION
Preventive vaccination offers the most efficient solution aimed to decrease the COVID-19 incidence and mortality. Vaccines based on viral vectors, self-replicating RNA, recombinant and native viral antigens are widely used for prevention of the novel coronavirus infection [1–5]. These platforms are efficient for development of vaccines that can induce protective immune responses. The main downsides of such vaccines are relatively short-term immune responses, an incomplete range of viral antigens, fast emergence of mutant viruses evading the post-vaccination immunity, and high manufacturing costs. In spite of the unprecedented epidemic control measures and wide use of vaccines against COVID-19, the pandemic spread of the SARS-CoV-2 coronavirus continues even in countries having high vaccination coverage1. New SARS-CoV-2 strains of increased epidemiological significance are reported regularly [6–8]. From August to November 2021, the Delta (B.1.617.2) variant that superseded Alpha, Beta, and Gamma variants accounted for 95% in the global incidence structure [9]. The Delta variant is highly contagious and is less efficiently neutralized by antisera obtained from recovered COVID 19 patients who had been infected with other variants of the virus [10–12]. November 2021 started with the rapid worldwide spread of another variant of SARS-CoV-2 – Omicron (B.1.1.529), which became dominant by February 2022, accounting for more than 95% among the strains identified by sequencing2. The Omicron variant has several deletions in the genome and more than 30 amino acid substitutions in the S protein, which resulted an enhanced binding affinity to the host ACE2-receptor and, consequently, increased transmissibility and a better ability to escape from neutralizing antibodies [13– 18]. Bowen et al. [14] have found that the neutralizing activity of sera from recovered patients and individuals vaccinated with different vaccines against COVID-19: mRNA-1273 (Moderna), BNT162b2 (Pfizer/BioNTech), COVID-19 Vaccine AstraZeneca (AstraZeneca), Sputnik V (Gamaleya Research Institute of Epidemiology and Microbiology), Novavax COVID-19 vaccine (Novavax), BBIP-CorV (Sinopharm), Ad26.COV2.S (Johnson & Johnson) is decreased toward two Omicron lineages – BA.1 and BA.2. The sera from patients recovered after infection with other variants of the virus has decreased neutralizing activity toward the Omicron variant [15]. The neutralizing activity of sera from people vaccinated with CoronaVac (Sinovac Biotech Ltd.) was significantly reduced or absent toward the Omicron variant [13][16]. Monoclonal antibodies, which are extensively used in COVID-19 treatment, are less effective toward the Omicron variant [17][18].
Undoubtedly, studies on vaccines demonstrating high protective activity toward a wide range of antigenic variants of SARS-CoV-2 are of critical importance. Live vaccines are among vaccines capable of inducing the immune response both to structural and non-structural viral proteins and activating not only the humoral, but also cell-mediated immunity. Multiple studies have demonstrated that the adaptation of viruses to growth at sub-optimal low temperatures leads to generation of a temperature-sensitive (ts) phenotype (decreased replication at 37ºC or above), which is associated with virulence attenuation in the normal host [19]. The resulting cold-adapted (ca) attenuated virus provides safe and effective protection against infection with the wild-type virus in immunized individuals [19]. Therefore, the aim of the study was to obtain ca-variants of SARS-CoV-2 and to provide their biological characterization.
MATERIALS AND METHODS
The virus and cell culture. The study was performed using the SARS-CoV-2 laboratory strain – Dubrovka (GenBank accession number: MW514307.1) [20] and its variants: Dubrovka-37, Dubrovka-ca, Dubrovka-ca-B4, Dubrovka-ca-D2 (GenBank accession numbers: ON380441.1, ON040960.1, ON059701.1, and ON040961.1, respectively). Vero CCL81 (ATCC) African green monkey kidney epithelial cells (further referred to as Vero cells) and Calu-3 HTB-55 (ATCC) human lung cancer cell culture (further referred to as Calu-3 cells) were used for virus culturing and experimental infection. The cells were cultured at 37ºC in the DMEM medium based on Earle’s buffer (PanEco) with 5% fetal calf serum (Gibco), 300 µg/ml L-glutamine (PanEco), 40 µg/ml gentamicin (PanEco) with 5% CO2. The three-day monolayer of Vero or Calu-3 cells was infected with SARS-CoV-2 at preferred multiplicity of infection (MOI). The virus adsorption was performed in a CO2 incubator for 60 min; then maintenance medium (DMEM, 300 µg/ml L-glutamine, 40 µg/ml gentamicin) was added, and the cells were incubated at 23– 39ºC for 3–8 days (depending on the virus variant and the purpose of the test) with 5% CO2. To analyze the kinetics of virus reproduction, culture liquid samples were collected daily for 4-8 days and stored at –80ºC till titration or quantitative real-time reverse transcription-polymerase chain reaction (real-time RT-PCR).
Animals. The study was performed using 36 golden Syrian female hamsters weighing 40–50 g (Nursery for Laboratory animals of the Institute of Bioorganic Chemistry of the Russian Academy of Sciences). The animals were randomly divided into 4 groups (n = 9), including three groups intended for infection with SARS-CoV-2 variants and the control group of non-infected animals. Authors confirm compliance with institutional and national standards for the use of laboratory animals in accordance with «Consensus Author Guidelines for Animal Use» (IAVES, 23 July 2010). The research protocol was approved by the Ethics Committee of the I.I. Mechnikov Research Institute of Vaccines and Sera (Protocol No. 2, May 24, 2021).
Virus titration. The SARS-CoV-2 titer was measured by the endpoint of the displayed cytopathic effect (CPE) in the Vero cell culture. The serial ten-fold dilutions of the virus in the maintenance medium were added to the wells of the 96-well plate and incubated for 5 days with 5% CO2 at 37ºC (ca-variants - at 30ºC). The titration results were assessed visually by microscopic examination of the cell monolayer for the presence of typical CPE on the 5th day after the infection (cell rounding and partial detachment of cells from the monolayer). The virus titer was calculated by the Ramakrishnan method [21] and expressed as lg TCID50/ml.
Quantification of SARS-CoV-2 RNA. The viral RNA was extracted using two techniques: The MagnoPrime Uni commercial reagent kit for DNA/RNA extraction from biological material (NextBio) in accordance with the manufacturer’s instruction or the Triton X-100 reagent kit. In the latter case, 10 µl of 4.5% Triton X-100 solution was added to 100 µl virus-containing culture liquid; the resulting mixture was refrigerated. After defrosting, the specimen was mixed, ten-fold diluted with RNase-free water and immediately put through real-time RT-PCR (the dilution factor of 10 was used for calculation of the viral RNA concentration).
To detect viral RNA by real-time RT-PCR, we used primers and the probe to the SARS-CoV-2 nucleocapsid N gene: COVID-19-N-F, COVID-19-N-R, COVID-19-N-P (Table) [22]. To perform real-time RTPCR, we used the reagent kit "2.5× reaction mix for real-time PCR with Taq DNA polymerase" and M-MLV reverse transcriptase (Syntol). The reaction mix of 25 µl contained 10 pmol of each primer and 5 pmol of the probe, Taq DNA polymerase, 30 units of reverse transcriptase. The temperature and time parameters were as follows: 45ºC — 10 min (1 cycle); 95ºC — 5 min (1 cycle); 95ºC — 5 sec, 55ºC — 45 sec (45 cycles). The reaction was performed in a DTprime thermocycler (DNA-Technology). All the primers and probes were produced by Syntol. To build the calibration graph, we used specimens obtained from serial ten-fold dilutions of synthetic oligonucleotide COVN-PC (Table) with the specified concentration.
Sequences of primers, probe, and oligonucleotide used in the tests
Name | Sequence 5’-3’ | Application | Source |
COVID-19-N-F | GCGTTCTTCGGAATGTCG | Forward primer | [22] |
COVID-19-N-R | TTGGATCTTTGTCATCCAATTTG | Reverse primer |
|
COVID-19-N-P | FAM-AACGTGGTTGACCTACACAGGT-BHQ1 | Probe |
|
COVN-PC | GCGTTCTTCGGAATGTCGCGCATTGGCATGGAAGTCACACCTTCGGGAA CGTGGTTGACCTACACAGGTGCCATCAAATTGGATGACAAAGATCCAA | Calibration sample | In-house design |
Sequencing of coronavirus genome. To receive a pool of amplicons for the subsequent whole-genome sequencing, we used the NEBNext® ARTIC SARSCoV-2 library preparation kit (Oxford Nanopore Technologies) (New England Biolabs). The kit is designed for whole-genome sequencing of SARS-CoV-2 in accordance with the SARS-CoV-2 McGill Nanopore sequencing protocol SuperScript IV_42C_ArticV3 [23]. To prepare the pool, we used Ligation Sequencing kit 1D and Native Barcoding Kit 1D kits (Oxford Nanopore Technologies). The sequencing was conducted in the Flow Cell R9.4 using the MinKNOW software (Oxford Nanopore Technologies). The genome was assembled using the Minimap2 v. 2.24 program3.
SARS-CoV-2 inactivation by ultraviolet (UV) radiation. The culture liquid from flasks with Vero cells was collected 72 hours after the infection with the virus; then the liquid was clarified by centrifugation at 4,000 rpm and titrated. The virus was inactivated by ultraviolet light (λ = 253.7 nm) using the TUV 30W/ G30 T8 germicidal lamp (Philips). The 150 mm-diameter Petri dish with the 50 ml of viral material was placed under the lamp at a distance of 30 cm and irradiated for 4 min; the liquid was stirred three times at regular intervals. The virus inactivation was confirmed by 3 consecutive "blind" passages of the irradiated viral material on Vero cell culture, including CPE and viral RNA concentration monitoring at each passage level.
Analysis of antigenic properties of UV-inactivated SARS-CoV-2. The dilutions of UV-inactivated SARS-CoV-2 were analyzed by the immunochromatography test using the SARS-CoV-2 Rapid Antigen Test reagent kit (SD Biosensor Inc.) in accordance with the user’s manual.
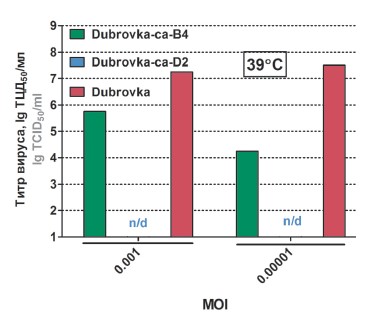
Identification of the ts-phenotype of SARSCoV-2 ca-variants. The Vero cells were infected with ca-variants of SARS-CoV-2 and the Dubrovka strain at MOI 0.001 and 0.00001 and incubated at 37ºC and 39ºC with 5% CO2 for 3 days. Samples of the culture liquid were collected daily and stored at –80ºC until the examination. The collected samples were used to measure the virus titer and viral RNA concentration. The difference in the virus titer or viral RNA concentration by 4.0 lg and greater compared to the infection with the Dubrovka strain was indicative of the presence of the ts-phenotype in the virus.
Identification of attenuation (att) phenotype of SARS-CoV-2 ca-variants. The Syrian hamsters were infected intranasally with the Dubrovka strain and ca-variants of the virus at a dose of 4.0 lg TCID50 (n = 9 in each group). The animals were examined daily, and their body weight was checked every 2 days. Four days after they had been infected, 4 hamsters from each group were euthanized; their lungs and brains were extracted, homogenized and stored at –80ºC until the examination. The health of the other animals was monitored, and their weight was checked for 8 days after they had been infected. The organ homogenates were used to measure the virus titer and viral RNA concentration. Significant differences in the weight, virus titer, or viral RNA concentration in the lungs and brain compared to the infection with the Dubrovka strain were indicative of the presence of the att-phenotype in the virus.
Transmission electron microscopy (TEM). Specimens of the ultraviolet-inactivated viral material were applied to TEM grids with carbon films (Ted Pella Carbon Type B, 300 mesh) and negatively contrasted with 1% uranyl acetate. The TEM images were received using a JEM-2100, 200 kV electron microscope (Jeol) equipped with a Gatan Orius SC200D (2k × 2k) camera.
Statistical analysis of the data. The statistical analysis of the data was performed using the Graphpad Prism v.5.03 software. The significance of differences was assessed by the Mann–Whitney U test with a 95% confidence interval.
Safety requirements. All the tests on SARS-CoV-2 were conducted in compliance with the requirements of the sanitary rules and regulations SanPiN 3.3686-21 in the biosafety level 3 laboratory.
RESULTS
Obtaining cold-adapted variants of SARS-CoV-2 The study was performed using the laboratory strain of SARS-CoV-2 – Dubrovka, which had been previously analyzed at the Mechnikov Research Institute for Vaccines and Sera. The Dubrovka strain was obtained in summer 2020, being isolated from the clinical sample collected from the patient with the confirmed diagnosis of COVID-19 and grown in the Vero cell culture. The virus identification was performed using real-time RT-PCR, the neutralization test with sera from the patients recovered from COVID-19, and whole-genome sequencing (GenBank accession number MW514307.1), which confirmed that the isolate belonged to the Severe acute respiratory syndrome-related coronavirus (SARS-CoV-2, clade GR according to the GISAID classification, lineage B.1.1.317 according to the PANGOLIN classification) [20]. The distinctive feature of the Dubrovka strain is that it has a 27 nt deletion in the S gene (9 amino acids from 68 to 76 aa — YMSLGPMVL) compared to the S gene of the Wuhan-Hu-1 strain (GenBank accession number NC_045512.2) [20]. All the variants of the Dubrovka strain, which were obtained during this study, had this deletion.
To study the adaption characteristics of SARSCoV-2, the Dubrovka strain was passaged for a long time in the Vero cell culture at the constant temperature of 37ºC or at the temperature that was gradually decreased to 23ºC during 42 passages. The obtained variants of the virus were called Dubrovka-37 and Dubrovka-ca (cold-adapted), respectively (Fig. 1). The Dubrovka-ca variant was obtained through the following process: 10 passages at 37ºC; then the temperature was decreased by 1ºC every 2 passages; the final 6 passages were performed at 23ºC (the total number of passages was 42). Then, using three-fold limiting dilution cloning at 23ºC, based on the Dubrovka-ca variant, we received two clones – B4 and D2 (further referred to as Dubrovka-ca-B4 and Dubrovka-ca-D2 variants).
Fig. 1. The schematic diagram of SARS-CoV-2 adaptationto the Vero cell culture and growth at low temperature.
Whole-genome sequences (GenBank accession numbers ON380441.1, ON040960.1, ON059701.1, and ON040961.1, respectively) were identified for variants of the Dubrovka strain: Dubrovka-37, Dubrovka-ca, Dubrovka-ca-B4, and Dubrovka-ca-D2. The primary analysis of genomes of different variants of the Dubrovka strain detected multiple nucleotide substitutions, most of which were nonsynonymous (resulted in amino acid substitution). After the continued adaptation to the Vero cell culture at 37ºC, the genome of the Dubrovka-37 variant had 7 nucleotide substitutions, 5 of which were nonsynonymous. The cold adaptation in the Vero cell culture caused 17 nucleotide substitutions in the genome of the Dubrovka-ca variant; 16 substitutions were nonsynonymous. At the same time, 16 and 20 nucleotide substitutions were detected in the genomes of clones of Dubrovka-ca-B4 and Dubrovka-ca-D2 ca-variants, causing 14 and 17 amino acid substitutions, respectively. The largest number of nonsynonymous substitutions was located in the S gene: 2 — in the Dubrovka-37 genome, 5 — Dubrovka-ca, 6 — Dubrovka-ca-B4, 7 — Dubrovka-ca-D2. Interestingly, in the genome of the Dubrovka-ca-D2 variant having the ts-phenotype, out of 20 nucleotide substitutions, 11 were unique in respect of Dubrovka-37, Dubrovka-ca, and Dubrovka-ca-B4; 9 of them caused amino acid substitutions.
PHENOTYPICAL CHARACTERIZATION OF SARS-COV-2 VARIANTS
During passages in the Vero cell culture at 37ºC, the virus titer increased (from 4.3 lg TCID50/ml in the 2nd passage to 9.0 lg TCID50/ml in the 30th passage), and CPE was becoming more pronounced. While after the infection with the virus of the 2nd passage, the survivability of the Vero cells was 92% on the 5the day after the infection, it went down to the minimum level (2-4%) by the 14th passage [20]. During the cold adaptation process, the time of the CPE development increased from 2–3 days at 37ºC to 5–7 days after the infection at 23ºC. The infection with the Dubrovka-ca variant produced CPE manifested in disruption of the monolayer integrity, clusters of rounded cells without their detaching from the flask surface (Fig. 2).
Fig. 2. Cytopathic effect of the Dubrovka-ca strain in the Vero cell culture at 23ºC (the 7th day after the infection). a — non-infected cells; b — Dubrovka-ca. MOI 0.001.
The Dubrovka-ca variant replicated much more slowly at 23ºC compared to the parent Dubrovka strain at its optimal temperature of 37ºC. Therefore, the cells were infected with a larger dose of the Dubrovka-ca variant and extended the incubation time. While the peak of replication of the Dubrovka strain (17th passage) at 37ºC (MOI 0.00001) was observed on the 2nd day, reaching 9.0 lg TCID50/ml, the replication of the Dubrovka-ca variant at 23ºC (MOI 0.001) reached its peak on the 7th day, reaching 8.0 lg TCID50/ml (Fig. 3). The viral replication was accompanied by accumulation of the viral RNA in the culture liquid (Fig. 3).
Fig. 3. Kinetics of virus replication and viral RNA accumulation for the Dubrovka strain (at 37⁰C) and the Dubrovka-ca variant (at 23⁰C) in Vero cell culture.The results of 2 independent tests are presented as mean values. The infection with the Dubrovka strain was performed at MOI 0.00001, the infection with the Dubrovka-ca variant — at MOI 0.001.
The Dubrovka-37 variant did not replicate in the Vero cell culture at 23ºC, while the Dubrovka-ca, Dubrovka-ca-B4, and Dubrovka-ca-D2 variants on the 7th day reached the titer of 4.5–8.0 TCID50/ml, depending on MOI.
Using the immunochromatographic test, the SARS-CoV-2 antigen was detected in all the UV inactivated virus variants — Dubrovka, Dubrovka-ca-B4, and Dubrovka-ca-D2. The TEM examination also detected virus-like particles having morpho diagnostic signs of the coronavirus: the virions had a rounded shape and had distinctive spikes of 12–15 nm on the envelope (S-protein trimers) (Fig. 4). The virion was 90–110 nm in diameter. The shape and size of the obtained virus-like particles matched the micrograph images of SARS-CoV-2, which had been made earlier [5][24].
Fig. 4. Electron microphotography of UV inactivated variants of SARS-CoV-2. a — Dubrovka; b — Dubrovka-ca-B4; c — Dubrovka-ca-D2. TEM. Negative contrasting with 1% uranyl acetate.The arrow shows S-protein trimers on the surface of the coronavirus. The scale bar — 100 nm.
The obtained clones of the Dubrovka-ca variant were examined for the presence of the temperature-sensitive (ts)-phenotype, which demonstrates the inability of the virus to replicate effectively at 37ºC or 39ºC. The replication intensity of Dubrovka-ca-B4 and Dubrovka-ca-D2 clones (MOI 0,001) at the Vero cell culture temperature of 37ºC was high and did not differ significantly from that of the Dubrovka strain (Fig. 5). At the culture temperature of 39ºC, the Dubrovka-ca-D2 variant did not replicate (Fig. 6), and the viral RNA concentration in the culture liquid was 4.0–6.0 lg lower compared to the Dubrovka strain and Dubrovka-ca-B4 variant (Fig. 5). Thus, it has been found that the Dubrovka-ca-D2 variant has a distinct ts-phenotype. The Dubrovka-ca-B4 variant also had signs of the ts-phenotype, though only at low MOI (0.00001) and the temperature of 39ºC – on the 3rd day the difference in the virus titer was 3.0 lg compared to the Dubrovka strain (Fig. 5).
Fig. 5. Accumulation of the viral RNA in the Vero cell culture after the infection with the Dubrovka strain and Dubrovka-ca-B4 and Dubrovka-ca-D2 variants at the culture temperature of 37ºC or 39ºC.The cells were infected at MOI = 0.001; samples of the culture liquid were collected daily, and the concentration of the viral RNA was measured. The results of 2 independent tests are presented as mean values.
Fig. 6. The virus titer on the 3rd day after the Vero cell culture had been infected with the Dubrovka strain and Dubrovka-ca-B4 and Dubrovka-ca-D2 variants; at the culture temperature of 39ºC and different MOI.The cells were infected with virus variants, and the virus titer was measured in the culture liquid 72 hours after the infection. The results of 2 independent tests are presented as mean values. n/d — not detected.
The Dubrovka-37 and Dubrovka-ca-B4 variants adapted throughout more than 40 passages in the monkey kidney Vero cell culture lost their ability to replicate in the Calu-3 human lung cancer cell culture. The Dubrovka-ca-D2 variant replicated in Calu-3 cells, though significantly more slowly than the Dubrovka strain (Fig. 7).
Fig. 7. Concentration of the viral RNA in Calu-3 cells infected with SARS-CoV-2 variants, the 3rd day after the infection, at MOI 0.001.1 — Dubrovka strain (the 2nd passage); 2 — Dubrovka-ca-B4; 3 — Dubrovka-ca-D2; 4 — Dubrovka-37. The results of 2 independent tests are presented as mean values.
The experimental intranasal infection of hamsters was performed to detect the attenuation (att) phenotype of ca-variants of SARS-CoV-2. The hamsters infected with ca-variants of SARS-CoV-2 did had no body weight loss and changes in the behavior compared to the negative control group. On the other hand, the infection with the virulent virus (the Dubrovka strain) caused a significant delay in the weight gain, and on the 2nd day after the infection it was 8.2%, on the 4th day — 13.4%, on the 6th day — 10.5% (p < 0.05), while on the 8th day the difference was insignificant (Fig. 8). The animals infected with the virulent strain demonstrated loss of appetite, fatiguem and drowsiness on the 2nd–6th day.
Fig. 8. Kinetics of the weight of hamsters infected intranasally with the Dubrovka strain and Dubrovka-ca-B4 and Dubrovka-ca-D2 variants.From the 0th to the 4th day — n = 9 per group; from the 6th to the 8th day — n = 5 per group. The infective dose — 4.0 lg TCID50. K– — non-infected hamsters.
On the 4th day after the infection with virus ca-variants, the viral RNA concentration in the animals’ lungs and brain was significantly lower compared to the concentration observed in the control group infected with the virulent Dubrovka strain (Fig. 9). The lowest concentration of the viral RNA in the organs was observed after the infection with the Dubrovka-ca-D2 variant: in lungs – 6.5 lg RNA copies/ml, in the brain – 3.3 lg RNA copies/ml, being by 1.6 and 3.2 lg lower than in the control group (p< 0.05).
Fig. 9. Concentration of the viral RNA in lung and brain homogenates from hamsters infected intranasally with the Dubrovka strain and Dubrovka-ca-B4 and Dubrovka-ca-D2 variants, 4th day after the infection.n = 4 per group. K– — non-infected hamsters.
On the 4th day after the infection with virus ca-variants, the virus titer in animals’ lung homogenates was 5.0 lg TCID50/ml or by 1.2 lg lower than in the control group (p < 0.05) (Fig. 10). The titration did not detect the infectious virus in the brain on the 4th day after the infection with ca-variants, while after the infection with the Dubrovka strain, the virus titer in the brain homogenates reached 5.0 lg TCID50/ml (Fig. 10). Note that the organ homogenates used for virus titration in 1 : 10 and 1 : 100 dilutions were toxic for cells, making it difficult to measure the viral CPE and reducing the titration sensitivity.
Fig. 10. The virus titer in lung and brain homogenates from hamsters infected intranasally with the Dubrovka strain and Dubrovka-ca-B4 and Dubrovka-ca-D2 variants, the 4th day after the infection.n = 4 per group. K– — non-infected hamsters.
DISCUSSION
The wide use of live virus vaccines included in national immunization schedules resulted in global eradication of smallpox and pushed such diseases as measles, rubella, chickenpox, mumps, and poliomyelitis to the brink of extinction in developed countries [25]. The virus strains used in development of most of the live virus vaccines were obtained by attenuation of wild variants of the respective viruses through adaptation to growth at low temperatures and/or in animal cells [25][26]. Numerous studies provided evidence that human and animal viruses can be adapted to growth at sub-optimal low temperatures [19]. Almost all cases demonstrated correlation between the temperature sensitivity acquired by these viruses in the tissue culture and the attenuation in the normal host – an animal or a human [19]. Tests demonstrated that cold adaptation can be used to produce an attenuated virus, which, when used for immunization, provides safe and effective protection against infection with the wild-type virus [19]. The seasonal live attenuated intranasal influenza vaccines developed in the Soviet Union and the United States [27–29] have significant advantages over inactivated vaccines, as they induce systemic, mucosal, and cell-mediated immunity, provide extensive cross-protection, and are easy to use. The use of live virus vaccines is justified not only by their high immunological efficacy, but also by their cost effectiveness resulting in low manufacturing costs [25].
In the meantime, based on the WHO data as of 13/5/2022, out of 153 COVID-19 vaccines approved and tested through clinical trials, only 2 (1.3%) vaccines are based on live attenuated strains: COVI-VAC (Codagenix/Serum Institute of India, India) and MV014-212 (Meissa Vaccines, Inc., United States)4. Both vaccines are intranasal. The strains used in these vaccines were attenuated by codon pair deoptimization.
Our study demonstrated that SARS-CoV-2 can be adapted to growth at the temperature of 23ºC, which is non-permissive for the wild-type virus, to produce ts-mutants. The obtained ca-variants of the virus — Dubrovka-ca-B4 and Dubrovka-ca D2 — had significant genomic differences compared to the parent Dubrovka strain; they replicated effectively at 23ºC; however, only the Dubrovka-ca-D2 variant had ts-phenotype, i.e. it did not replicate at 39ºC. Furthermore, the Dubrovka-ca D2 and Dubrovka-ca-B4 clones adapted to the monkey kidney Vero cell culture replicated significantly more slowly than the wild-type strain at 37ºC in the human lung cancer Calu-3 cell culture, which, together with the ts-phenotype, can serve as a marker of virus attenuation in human. Therefore, we have grounds to assume that both the Dubrovka-ca-D2 clone, which has the ts-phenotype, and the Dubrovka-ca-B4 clone, which does not have the ts-phenotype, are characterized by low virulence, i.e. are attenuated.
In the test performed using Syrian hamsters, the animal model for COVID-19 confirmed the assumption about the attenuation of ca-variants of the Dubrovka strain. The hamsters infected intranasally with the Dubrovka-ca-B4 and Dubrovka-ca-D2 variants did not have any loss of appetite, fatigue, drowsiness, or slow weight gain compared to the hamsters infected with virulent Dubrovka strain. In the lungs and brain of the animals infected with ca-variants, the viral RNA concentration and the infectious virus titers were 1.2–3.3 lg lower compared to the virulent strain; the lowest reproductive activity in vivo was demonstrated by the ts+ Dubrovka-ca-D2 clone. Note that in the brain of hamsters infected with ca-variants, the infectious virus was not detected, while in the hamsters infected with the virulent Dubrovka strain, the virus titer reached 5.0 lg TCID50/ml of the homogenate. Considering the neurovirulence of SARS-CoV-2 in humans, the decrease in the replication activity of virus ca-variants in the brain of hamsters infected intranasally decreases the risk of neurological damage in vivo and is an important marker of the virus attenuation. Thus, the obtained ca-variants of Dubrovka-ca-B4 and Dubrovka-ca-D2 have a distinct att-phenotype for Syrian hamsters and offer promising opportunities for the further studies as candidate vaccine strains for development of a live attenuated vaccine against COVID-19.
It should be noted that the attenuation phenotype of virus ca-variants was obtained using Syrian hamsters and should be studied further on other models. The data on the virus virulence, which were obtained using animal models, cannot be automatically extrapolated to humans. Preclinical trials using animal models provide only an approximate idea about safety of clinical use and human susceptibility to attenuated strains of the virus. Furthermore, the possible reversion of the vaccine strain virulence due to point mutations or recombinations can be a serious risk factor in using live attenuated vaccines. It calls for further studies of the genetic stability of SARS-CoV-2 ca-variants and the associated stability of the att-phenotype.
Scientific publications describe SARS-CoV-2 castrains with the ts-phenotype and the att-phenotype, which when administered intranasally, were able to induce a protective immune response against the virulent strain SARS-CoV-2 in immunized animals (Syrian hamsters or transgenic mice hACE-2 (K18-hACE2) [30–32]. In the above studies, different techniques were used to obtain ts+ strains of SARS-CoV-2. Seo et al. [30] used the approach similar to the technique we used in our study — continued passaging at the temperature gradually decreasing from 37ºC to 22ºC in Vero cells. In their study, Okamura et al. used the SARSCoV-2 clinical isolate to generate a large library of 659 clones containing random mutations; these clones were used to select variants causing CPE in the cell culture at 32ºC rather than at 37ºC [32]. When producing a vaccine strain, the virus attenuation must provide balance between the attenuation of virulence and the retained ability to induce a protective immune response. Experimental tests proved that protective activity can be preserved in attenuated ts-mutants of SARS-CoV-2 [30][32]. Therefore, the protective activity of the Dubrovka-ca-B4 and Dubrovka-ca-D2 variants obtained using the animal model for COVID-19 should be studied further.
CONCLUSION
The obtained attenuated ca-variants of SARSCoV-2 — Dubrovka-ca-B4 and Dubrovka-ca-D2 — should be studied further as candidate vaccine strains for a live attenuated vaccine against COVID-19.
1. WHO Coronavirus (COVID-19) Dashboard. URL: https://covid19.who.int (дата обращения: 13.05.2022).
2. The GISAID Initiative. URL: https://www.gisaid.org (дата обращения: 13.05.2022)
3. URL: https://github.com/lh3/minimap2
4. R&D Blue Print. World Health Organization. COVID-19 vaccine tracker and landscape. URL: https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines (дата обращения: 13.05.2022).
About the authors
Evgeny B. Faizuloev
I.I. Mechnikov Research Institute of Vaccines and Sera
Author for correspondence.
Email: faizuloev@mail.ru
ORCID iD: 0000-0001-7385-5083
Cand. Sci. (Biol.), Head, Laboratory of molecular virology
Russian Federation, MoscowEkaterina R. Korchevaya
I.I. Mechnikov Research Institute of Vaccines and Sera
Email: faizuloev@mail.ru
ORCID iD: 0000-0002-6417-3301
junior researcher, Laboratory of molecular virology
Russian Federation, MoscowAnastasiia V. Gracheva
I.I. Mechnikov Research Institute of Vaccines and Sera
Email: faizuloev@mail.ru
ORCID iD: 0000-0001-8428-4482
junior researcher, Laboratory of molecular virology
Russian Federation, MoscowRoman V. Samoilikov
I.I. Mechnikov Research Institute of Vaccines and Sera
Email: faizuloev@mail.ru
ORCID iD: 0000-0001-6405-1390
junior researcher, Laboratory of molecular virology
Russian Federation, MoscowDaria I. Smirnova
I.I. Mechnikov Research Institute of Vaccines and Sera
Email: faizuloev@mail.ru
ORCID iD: 0000-0001-7325-0834
junior researcher, Laboratory of molecular virology
Russian Federation, MoscowOlga S. Sokolova
Lomonosov Moscow State University, Faculty of Biology
Email: faizuloev@mail.ru
ORCID iD: 0000-0003-4678-232X
D. Sci. (Biol.), Professor, Bioengineering department, Faculty of Biology
Russian Federation, MoscowGrigory S. Glukhov
Lomonosov Moscow State University, Faculty of Biology
Email: faizuloev@mail.ru
ORCID iD: 0000-0002-9540-8249
Cand. Sci. (Biol.), Associate Professor, Bioengineering department, Faculty of Biology
Russian Federation, MoscowAndrey V. Moiseenko
Lomonosov Moscow State University, Faculty of Biology
Email: faizuloev@mail.ru
ORCID iD: 0000-0003-1112-2356
leading engineer, Laboratory of electron microscopy, Faculty of Biology
Russian Federation, MoscowIrina A. Leneva
I.I. Mechnikov Research Institute of Vaccines and Sera
Email: faizuloev@mail.ru
ORCID iD: 0000-0002-7755-2714
D. Sci. (Biol.), Head, Laboratory of experimental virology
Russian Federation, MoscowFiraya G. Nagieva
I.I. Mechnikov Research Institute of Vaccines and Sera
Email: faizuloev@mail.ru
ORCID iD: 0000-0001-8204-4899
D. Sci. (Med.), Associate Professor, Head, Laboratory of hybrid cell cultures
Russian Federation, MoscowOksana A. Svitich
I.I. Mechnikov Research Institute of Vaccines and Sera; I.M. Sechenov First Moscow State Medical University (Sechenov University)
Email: faizuloev@mail.ru
ORCID iD: 0000-0003-1757-8389
D. Sci. (Med.), Professor, Corresponding Member of RAS, Head, Laboratory of molecular immunology, Director
Russian Federation, Moscow; MoscowVitaly V. Zverev
I.I. Mechnikov Research Institute of Vaccines and Sera; I.M. Sechenov First Moscow State Medical University (Sechenov University)
Email: faizuloev@mail.ru
ORCID iD: 0000-0001-5808-2246
D. Sci. (Biol.), Professor, Academician of RAS, Scientific director
Russian Federation, Moscow; MoscowReferences
- Francis A.I., Ghany S., Gilkes T., Umakanthan S. Review of COVID-19 vaccine subtypes, efficacy and geographical distributions. Postgrad. Med. J. 2022; 98(1159): 389-94. https://doi.org/10.1136/postgradmedj-2021-140654
- Marfe G., Perna S., Shukla A.K. Effectiveness of COVID-19 vaccines and their challenges (Review). Exp. Ther. Med. 2021; 22(6):1407. https://doi.org/10.3892/etm.2021.10843
- Marcelin J.R., Pettifor A., Janes H., Brown E.R., Kublin J.G., Stephenson K.E. COVID-19 vaccines and SARS-CoV-2 transmission in the era of new variants: A review and perspective. Open Forum Infect. Dis. 2022; 9(5): ofac124. https://doi.org/10.1093/ofid/ofac124
- Kandimalla R., Chakraborty P., Vallamkondu J., Chaudhary A., Samanta S., Reddy P.H., et al. Counting on COVID-19 vaccine: insights into the current strategies, progress and future challenges. Biomedicines. 2021; 9(11): 1740. https://doi.org/10.3390/biomedicines9111740
- Kozlovskaya L.I., Piniaeva A.N., Ignatyev G.M., Gordeychuk I.V., Volok V.P., Rogova Y.V., et al. Long-term humoral immunogenicity, safety and protective efficacy of inactivated vaccine against COVID-19 (CoviVac) in preclinical studies. Emerg. Microbes Infect. 2021; 10(1): 1790-806. https://doi.org/10.1080/22221751.2021.1971569
- Gómez-Carballa A., Pardo-Seco J., Bello X., Martinón-Torres F., Salas A. Superspreading in the emergence of COVID-19 variants. Trends Genet. 2021; 37(12): 1069-80. https://doi.org/10.1016/j.tig.2021.09.003
- Nikonova A.A., Faizuloev E.B., Gracheva A.V., Isakov I.Y., Zverev V.V. Genetic diversity and evolution of the biological features of the pandemic SARS-CoV-2. Acta Naturae. 2021; 13(3): 77-88. https://doi.org/10.32607/actanaturae.11337
- Choi J.Y., Smith D.M. SARS-CoV-2 variants of concern. Yonsei Med. J. 2021; 62(11): 961-8. https://doi.org/10.3349/ymj.2021.62.11.961
- Mathieu E., Ritchie H., Ortiz-Ospina E., Roser M., Hasell J., Appel C., et al. A global database of COVID-19 vaccinations. Nat. Hum. Behav. 2021; 5(7): 947-53. https://doi.org/10.1038/s41562-021-01122-8
- Dupont L., Snell L.B., Graham C., Seow J., Merrick B., Lechmere T., et al. Neutralizing antibody activity in convalescent sera from infection in humans with SARS-CoV-2 and variants of concern. Nat. Microbiol. 2021; 6(11): 1433-42. https://doi.org/10.1038/s41564-021-00974-0
- Tao K., Tzou PL., Nouhin J., Gupta R.K., de Oliveira T., Kosakovsky Pond S.L., et al. The biological and clinical significance of emerging SARS-CoV-2 variants. Nat. Rev. Genet. 2021; 22(12): 757-73. https://doi.org/10.1038/s41576-021-00408-x.
- Saito A., Irie T., Suzuki R., Maemura T., Nasser H., Uriu K., et al. Enhanced fusogenicity and pathogenicity of SARS-CoV-2 Delta P681R mutation. Nature. 2021; 602(7896): 300-6. https://doi.org/10.1038/s41586-021-04266-9
- Lu L., Mok B.W., Chen L.L., Chan J.M., Tsang O.T., Lam B.H., et al. Neutralization of SARS-CoV-2 Omicron variant by sera from BNT162b2 or Coronavac vaccine recipients. Clin. Infect. Dis. 2021; ciab1041. https://doi.org/10.1093/cid/ciab1041
- Bowen J.E., Sprouse K.R., Walls A.C., Mazzitelli I.G., et al. Omicron BA.1 and BA.2 neutralizing activity elicited by a comprehensive panel of human vaccines. bioRxiv. 2022. Preprint. https://doi.org/10.1101/2022.03.15.484542
- Dejnirattisai W., Huo J., Zhou D., Zahradník J., Supasa P., Liu C., et al. Omicron-B.1.1.529 leads to widespread escape from neutralizing antibody responses. bioRxiv. 2021. Preprint. https://doi.org/10.1101/2021.12.03.471045
- Wang Y., Ma Y., Xu Y., Liu J., Li X., Chen Y., et al. Resistance of SARS-CoV-2 Omicron variant to convalescent and CoronaVac vaccine plasma. Emerg. Microbes Infect. 2022; 11(1): 424-7. https://doi.org/10.1080/22221751.2022.2027219
- Sheward D.J., Kim C., Ehling R.A., Pankow A., Dopico X.C., Martin D.P., et al. Variable loss of antibody potency against SARS-CoV-2 B.1.1.529 (Omicron). bioRxiv. 2021. Preprint. https://doi.org/10.1101/2021.12.19.473354
- VanBlargan L.A., Errico J.M., Halfmann P.J., Zost S.J., Crowe J.E. Jr., Purcell L.A., et al. An infectious SARS-CoV-2 B.1.1.529 Omicron virus escapes neutralization by therapeutic monoclonal antibodies. Nat. Med. 2022; 28(3): 490-5. https://doi.org/10.1038/s41591-021-01678-y
- Maassab H.F., DeBorde D.C. Development and characterization of cold-adapted viruses for use as live virus vaccines. Vaccine. 1985; 3(5): 355-69. https://doi.org/10.1016/0264-410x(85)90124-0
- Грачёва А.В., Корчевая Е.Р., Кудряшова А.М., Борисова О.В., Петруша О.А., Смирнова Д.И. и др. Адаптация МТТ-теста для определения нейтрализующих антител к вирусу SARS-CoV-2. Журнал микробиологии, эпидемиологии и иммунобиологии. 2021; 98(3): 253-65. https://doi.org/10.36233/0372-9311-136
- Ramakrishnan M.A. Determination of 50% endpoint titer using a simple formula. World J. Virol. 2016; 5(2): 85-6. https://doi.org/10.5501/wjv.v5.i2.85
- Chan J.F., Yip C.C., To K.K., Tang T.H., Wong S.C., Leung K.H., et al. Improved molecular diagnosis of COVID-19 by the novel, highly sensitive and specific COVID-19-RdRp/Hel real-time reverse transcription-PCR assay validated in vitro and with clinical specimens. J. Clin. Microbiol. 2020; 58(5): e00310-20. https://doi.org/10.1128/JCM.00310-20
- Reiling S.J., Chen S.H., Roy A.M., Quick J., Ragoussis I. SARSCoV-2 McGill Nanopore sequencing protocol SuperScript IV_42C_ArticV3. Available at: https://www.protocols.io/view/sars-cov-2-mcgill-nanopore-sequencing-protocol-supq26g7b25klwz/v1
- Liu C., Mendonça L., Yang Y., Gao Y., Shen C., Liu J., et al. The architecture of inactivated SARS-CoV-2 with postfusion spikes revealed by Cryo-EM and Cryo-ET. Structure. 2020; 28(11): 1218-24.e4. https://doi.org/10.1016/j.str.2020.10.001
- Minor P.D. Live attenuated vaccines: Historical successes and current challenges. Virology. 2015; 479-480: 379-92. https://doi.org/10.1016/j.virol.2015.03.032
- Subbarao K. Live attenuated cold-adapted influenza vaccines. Cold Spring Harb. Perspect. Med. 2021; 11(9): a038653. https://doi.org/10.1101/cshperspect.a038653
- Alexandrova G.I., Smorodintsev A.A. Obtaining of an additionally attenuated vaccinating cryophilic influenza strain. Rev. Roum. Inframicrobiol. 1965; 2(3): 179-86.
- Ghendon Y.Z., Polezhaev F.I., Lisovskaya K.V., Medvedeva T.E., Alexandrova G.I., Klimov A.I. Recombinant cold-adapted attenuated influenza A vaccines for use in children: molecular genetic analysis of the cold-adapted donor and recombinants. Infect. Immun. 1984; 44: 730-3. https://doi.org/10.1128/IAI.44.3.730-733.1984
- Maassab H.F. Adaptation and growth characteristics of influenza virus at 25 C. Nature. 1967; 213(5076): 612-4. https://doi.org/10.1038/213612a0
- Seo S.H., Jang Y. Cold-adapted live attenuated SARS-Cov-2 vaccine completely protects human ACE2 transgenic mice from SARS-CoV-2 infection. Vaccines (Basel). 2020; 8(4): 584. https://doi.org/10.3390/vaccines8040584
- Okamura S., Ebina H. Could live attenuated vaccines better control COVID-19? Vaccine. 2021; 39(39): 5719-26. https://doi.org/10.1016/j.vaccine.2021.08.018
- Okamura S., Kashiwabara A., Suzuki H., Ueno S., Miyazato P., Takekawa S., et al. Live attenuated SARS-CoV-2 vaccine candidate: Protective immunity without serious lung lesions in Syrian hamsters. bioRxiv. 2021. Preprint. https://doi.org/10.1101/2021.02.15.430863
Supplementary files